Introduction
Administering the correct amount of oxygen to patients is a critical aspect of medical care, particularly in scenarios involving respiratory distress or chronic pulmonary disorders. Calculating the precise oxygen dosage ensures efficient treatment while minimizing risks associated with oxygen toxicity. This process involves understanding the patient's oxygen saturation levels, their respiratory rate, and the desired oxygen saturation target.
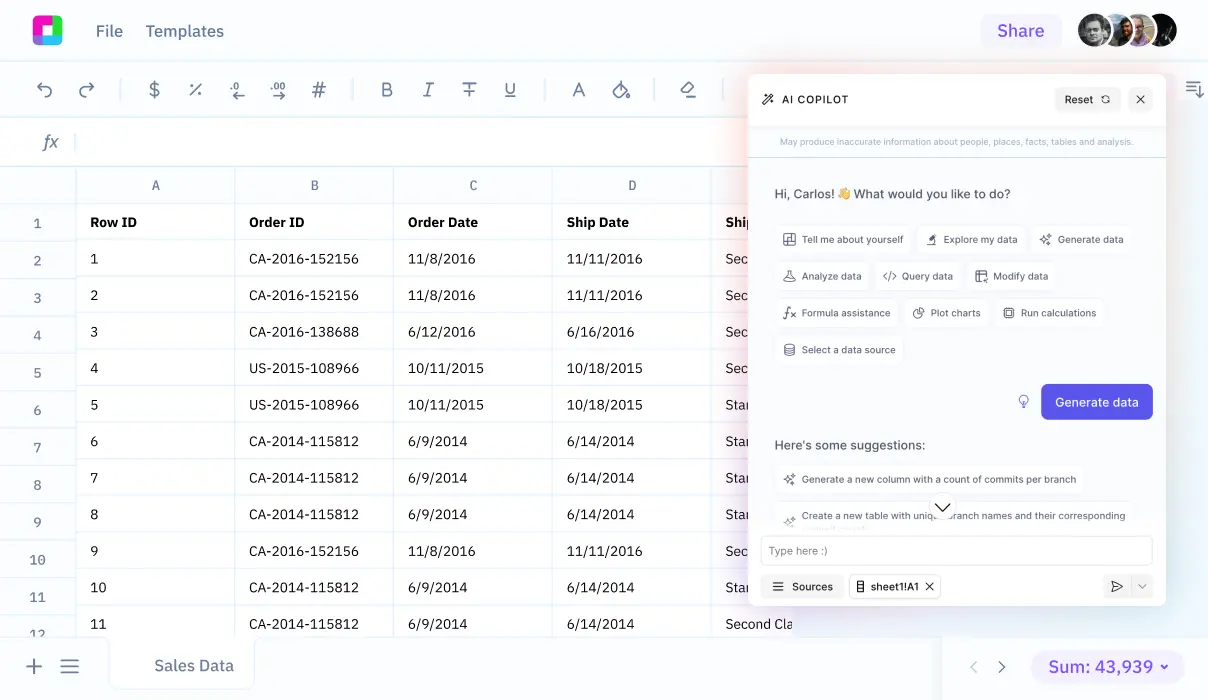
Navigating these calculations can be complex, requiring accurate input and considerations of several physiological parameters. Fortunately, technological tools like Sourcetable can streamline these calculations. Sourcetable's AI-powered spreadsheet assistant simplifies the process, helping healthcare providers make informed decisions quickly. We'll explore how Sourcetable facilitates this critical task and more. Try it at app.sourcetable.com/signup.
See how easy it is to oxygen dosage for a patient with Sourcetable
How to Calculate Oxygen for Patients
Understanding Patient Needs
Begin by consulting clinicians to assess the patient mix and disease burden, crucial for accurately determining oxygen needs in a medical setting. Understanding individual patient conditions, whether at rest or exercising, is vital as it influences oxygen requirements.
Calculating Minute Ventilation
Calculate the minute ventilation by multiplying the tidal volume (6-10 ml/kg) by the respiration rate. Measure this in liters per minute (L/min). This initial calculation aids in determining the volume of air inhaled and exhaled by a patient each minute.
Determining Peak Inspiratory Flow Rate
The peak inspiratory flow rate, measured in liters per second (L/s), is calculated next. This rate is essential to configure the subsequent adequate oxygen flow for therapy.
Oxygen Delivery Rate
Using the derived peak inspiratory flow rate, establish the appropriate oxygen delivery rate. This rate will vary depending on the patient's age, specific oxygen demand, and the method of oxygen administration being employed (e.g., mask or nasal prong).
Adjusting Flow Rate and Monitoring
Meticulously adjust the flow rate to maintain the patient's target SpO2, using the lowest flow rate necessary. Deploy pulse oximetry to prevent over-oxygenation, conserving oxygen while ensuring patient safety.
Special Considerations for Equipment
For environments like hospitals, consider utilizing duplex systems instead of large single plants. This arrangement can be more adaptable to varying demands and ensure continuous oxygen supply.
Estimating Overall Oxygen Needs for Facilities
For calculating oxygen needs across a healthcare facility, utilize the formula: [number of beds x 0.75 LPM] + [number of additional outlets (ICU, operating theatre, etc.) x 10 LPM] = Total LPM. This estimation helps in orchestrating the logistics of oxygen supply across various departments efficiently.
How to Calculate Oxygen Dosage for Patients
Initial Consultation and Assessment
Begin the oxygen dosage calculation by consulting clinicians to understand the patient mix and disease burden. This stage helps assess the demand for oxygen, especially if some clinicians lack training in respiratory care, which could influence oxygen consumption.
Determining Oxygen Delivery
Calculate the oxygen delivery (DO2) by considering the total oxygen content (CaO2) and cardiac output (CO). The formula DO2 = CaO2 * CO integrates oxygen content, which is a function of hemoglobin concentration ([Hb]) and oxygen saturation (SaO2), with cardiac output—calculated from stroke volume (SV) and heart rate (HR).
Prescribing and Administering Oxygen
Oxygen should be prescribed within a target saturation range, using hospital electronic prescribing systems (HEPMA) where available. Initially administer oxygen using a reservoir mask at a flow rate of 15L/minute. Subsequently, adjust the flow to achieve the target saturation of 94-98% in patients without risk of hypercapnic respiratory failure or 88-92% in those with this condition.
Oxygen Therapy Adjustments Based on ABG Analysis
After initial administration, perform an arterial blood gas (ABG) analysis. Adjust the oxygen flow based on ABG results to maintain the appropriate saturation levels, rechecking ABG as necessary depending on the patient's pCO2 and H+ levels.
Calculating Oxygen Dosage for Patients
Example 1: Standard Oxygen Therapy
Predict patient oxygen needs using a simple formula: FiO2 \times (Desired PaO2 / Current PaO2). For a patient needing an increase in PaO2 from 60mmHg to 80mmHg using an FiO2 of 0.21 (ambient air), calculate: 0.21 \times (80 / 60) \approx 0.28. Thus, set the oxygen flow to achieve an FiO2 of around 0.28.
Example 2: Oxygen Therapy for COPD
For COPD patients requiring controlled oxygen therapy, target a specific PaO2. If aiming for a PaO2 of 60mmHg from a current 50mmHg using an FiO2 of 0.24, apply the formula: 0.24 \times (60 / 50) = 0.288. Adjust the oxygen supply to maintain an FiO2 near 0.288, preventing hyperoxia risks.
Example 3: High-altitude Adjustment
Adjust oxygen needs for altitude. If a patient ascends to 3000 meters, reducing ambient FiO2 to approximately 0.16, and needs to maintain a normal PaO2 (say 75mmHg), recalculate: 0.16 \times (75 / 60) = 0.20. Increase supplemental oxygen to match this adjusted FiO2.
Example 4: Pediatric Oxygen Needs
Children have different metabolic rates and thus different oxygen needs. For a child with PaO2 of 75mmHg needing increase to 90mmHg, and starting FiO2 at 0.21, use the equation: 0.21 \times (90 / 75) = 0.252. Provide oxygen flow to reach the calculated FiO2 of approximately 0.25.
Explore the Power of Sourcetable for All Your Calculation Needs
Understanding how to make precise calculations in professional settings, such as healthcare, can dramatically impact outcomes. Sourcetable simplifies complex calculations, like determining how to calculate how much oxygen to give a patient, using its AI-driven capabilities.
Accurate Healthcare Calculations with Sourcetable
For healthcare professionals, ensuring the correct dosage of oxygen is critical. Sourcetable's AI assistant can seamlessly compute the necessary amount of oxygen for patients. Users simply input variables such as SpO_2 levels and patient weight, and Sourcetable provides accurate calculations. This feature not only saves time but also enhances patient safety by reducing human error.
Benefits for Education and Professional Use
Sourcetable is an indispensable tool for students and professionals alike. It offers detailed explanations in a chat interface of the calculations performed, making it an excellent resource for learning and review. Whether it's for studying or solving real-time problems at work, Sourcetable delivers precise calculations and insights right at your fingertips.
Embrace the efficiency and accuracy of Sourcetable for all your calculation needs, from daily tasks to critical healthcare decisions.
Use Cases for Calculating Oxygen Dosage for Patients
Pediatric Oxygen Delivery |
For pediatric patients, calculate oxygen flow rates based on whether nasal prongs with or without humidification are used. For infants under 2 years without humidification, use up to 2 LPM and for those over 2 years, up to 4 LPM. With humidification, these increase to 4 LPM for infants and 6 LPM for older children. This ensures safe oxygen levels without causing dryness or discomfort. |
Adult Patients with High Respiratory Rates |
In adult patients experiencing respiratory rates higher than 30 breaths per minute, increase the initially suggested maximal flow rate by a factor of 1.5 to 2. This adjustment helps to meet the elevated ventilatory demand, ensuring effective respiratory support during periods of intense respiratory distress. |
Adjusting Oxygen Dosage in Altitude Changes |
Utilize pulse oximetry to determine if supplemental oxygen is necessary when patients are exposed to high altitudes or during air travel. An altitude simulation test can confirm the safe oxygen saturation levels at approximately 8,000 feet, the common cabin pressure altitude in commercial flights. This is crucial for patients with compromised lung function. |
Calculating Oxygen Needs in Clinical Settings |
Engage with clinicians to understand the patient mix and disease burden in a facility. Use this data to calculate the overall oxygen demand, optimizing respiratory care and preventing over-oxygenation. Implement training for clinicians on the use of pulse oximeters, which help conserve oxygen while ensuring patient safety. |
Frequently Asked Questions
How do you calculate the flow rate of oxygen for a patient with a respiratory rate over 30 breaths per minute?
For patients with a respiratory rate of more than 30 breaths per minute, increase the flow rate by 1.5-2 times the maximum suggested on the Venturi mask packaging.
What factors should be considered when determining the oxygen therapy dosage for a patient?
The oxygen therapy dosage should be determined based on the medical condition of the patient, the results of pulmonary function tests, and the amount of oxygen needed to maintain healthy organ function or to make the patient feel good.
How should oxygen be prescribed to achieve a specific target saturation range?
Oxygen should be prescribed to achieve a target saturation range as recommended by the guideline. Patients should be monitored continuously to ensure they remain within this target range.
What is the procedure for adjusting oxygen therapy if the targeted oxygen saturation is not achieved?
If the target oxygen saturation is not reached, the oxygen delivery system should be checked for faults, and the therapy may need to be increased according to a written protocol. Blood gas measurements should be repeated if there is no improvement after 5-10 minutes of increased therapy.
How do you calculate total oxygen demand for a healthcare facility?
To calculate the total demand of oxygen for a healthcare facility, use the formula from the OGSI website: [# of beds x 0.75 LPM] + [# of other outlets (such as ICU, operating theatre, etc.) x 10 LPM] for the total liters per minute (LPM) and then multiply this by 2.
Conclusion
Calculating the correct amount of oxygen to administer to a patient is crucial for effective treatment and recovery. Understanding the importance of accurate dosing ensures that patients receive the optimal level of care.
Streamline Your Calculations with Sourcetable
Sourcetable, an AI-powered spreadsheet, enhances the efficiency and accuracy of medical calculations. Its intuitive interface allows healthcare professionals to easily compute vital parameters, such as the necessary oxygen flow rate, which can be expressed with the formula O_2\,flow\,rate = (Desired\,PaO_2 - PaO_2\,on\,room\,air) / FiO_2.
Test Your Calculations on AI-Generated Data
Before applying these calculations in real scenarios, you can test them on AI-generated data provided by Sourcetable. This feature helps in perfecting the calculations under various simulated conditions, ensuring readiness and reliability.
Explore the straightforward functionality of Sourcetable and improve your medical calculation capabilities today. You can try Sourcetable for free at app.sourcetable.com/signup.
Recommended Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.
- how to calculate how long an oxygen tank will last
- how to calculate ml/kg/day nicu
- how to calculate minute ventilation
- how to do dosage calculations
- how to calculate expiratory reserve volume
- how to calculate chemo dose
- how to calculate dose per kg body weight
- a nurse is calculating a client's fluid intake