Introduction
Accurately calculating chemotherapy dosages is crucial for safe and effective cancer treatment. The process involves considering factors like the patient's weight, body surface area (BSA), and the specific drug's characteristics. Precise calculations ensure that patients receive the optimal dose necessary for their treatment. This not only maximizes the therapeutic benefits but also minimizes potential side effects.
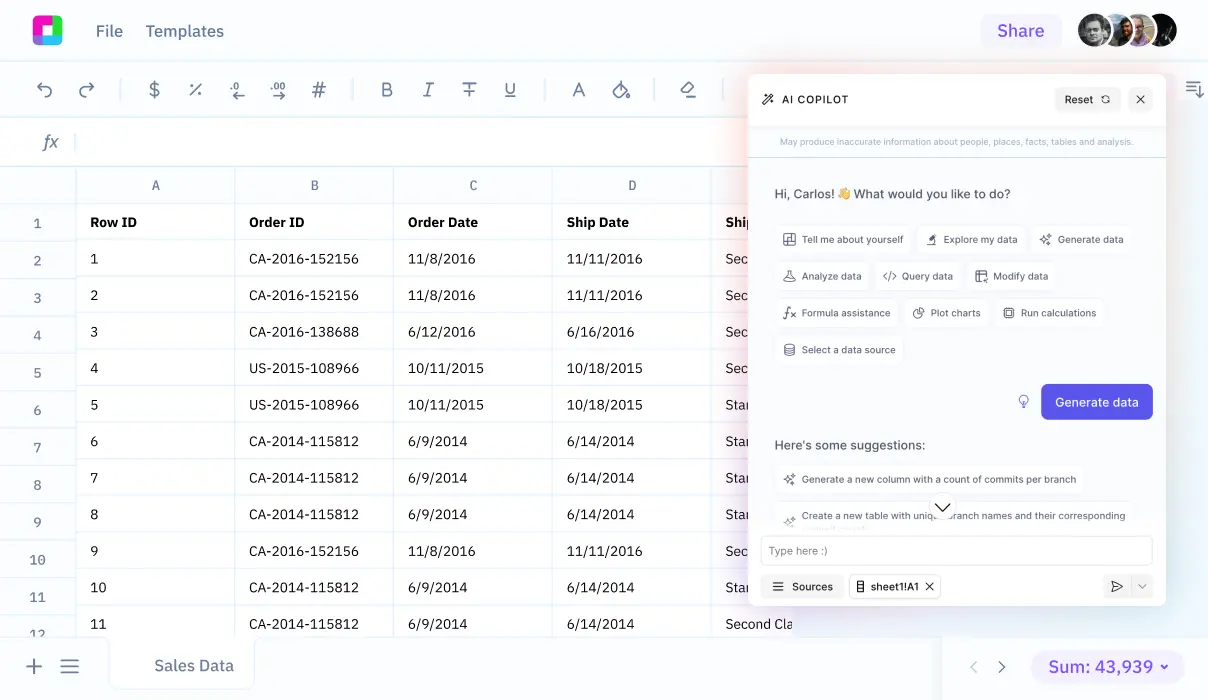
With technological advancements, tools like Sourcetable have revolutionized how healthcare professionals approach these calculations. By leveraging AI capabilities in its spreadsheet assistant, Sourcetable simplifies the complexity involved in calculating chemo doses. This guide will explore how Sourcetable lets you calculate chemo doses and more using its AI-powered spreadsheet assistant, which you can try at app.sourcetable.com/signup.
See how easy it is to chemo dose with Sourcetable
How to Calculate Chemo Dose
Understanding Chemotherapy Dose Calculation
Chemotherapy dosing requires accuracy due to high toxicity and a narrow therapeutic index of agents. Effective dose calculation hinges on the oncology team’s competency and the use of evidence-based formulas to mitigate medication errors.
Methods for Chemotherapy Dose Calculation
Two predominant methods are utilized: Body Surface Area (BSA) based dosing and fixed-dose guidelines. BSA is calculated using formulas like the Dubois Formula (Dubois Formula) and the Monteller Formula (Monteller Formula), which have been standard for adult dosing. However, limitations in predicting drug exposure by BSA have shifted some recommendations towards fixed-dosing implementation, particularly with agents like cisplatin and epirubicin wherein liver function tests might offer better indicators of drug handling.
Fixed Dose and Myelosuppression Based Adjustments
Fixed dosing can be independent of BSA and may instead focus on the patient's drug elimination capabilities, serving as a starting point or adjustment parameter. Myelosuppression levels, indicating marrow activity suppression due to the chemotherapy, provide a robust feedback mechanism for dose adjustment, enhancing the accuracy of dosing beyond what BSA-based calculations can offer.
Key Considerations for Accurate Dosing
Oncology teams must ensure safety and efficacy by verifying the dose calculations and understanding the dose-limiting toxicities of chemotherapeutic agents. Regular competency training and participation in safety verification processes are critical to maintain optimal dosing practices.
How to Calculate Chemo Dose
Understanding the Basics of Chemotherapy Dosing
Accurate chemotherapy dosing is critical to treatment efficacy and patient safety. The oncology team should master dose calculations, understand dose-limiting toxicities, and follow safety verification processes to ensure appropriate medication administration.
Methods of Chemo Dose Calculation
Chemotherapy dosage can be calculated using body surface area (BSA) or via pharmacokinetic profiles of drug elimination. Traditional BSA-based dosing employs formulas like the Dubois Formula, Dose = BSA Based Dose * 0.007184 * Height(cm)^0.725 * Weight(kg)^0.425, and the Mosteller Formula, BSA Based Dose x sqrt[(Height (cm) x Weight (kg)) / 3600]. However, this method has faced criticism for not accounting for individual variations in drug clearance and metabolism.
Considering Pharmacokinetics and Drug Elimination
For most accurate dosing, focus on pharmacokinetic methods that consider drug elimination and metabolic phenotypes. Factors such as genetic makeup, environmental factors, and individual health conditions like liver or renal function profoundly affect drug clearance rates, highlighting the limitations of BSA-based methods. For drugs like Carboplatin, dosage adjustment based on glomerular filtration rate (GFR) is effective.
Alternative Approaches to Dosage Calculation
Emerging techniques involve advanced body measurements and adjusting doses based on myelosuppression outcomes to enhance the precision of chemotherapy dosing. Utilization of 3D imaging and other advanced body measurement technologies is recommended to avoid underdosing or overdosing, thus optimizing therapeutic outcomes and reducing toxicity.
Conclusion
While BSA has been a common basis for calculating chemotherapy doses, its reliability is questionable for modern, diverse populations with varying body compositions. More accurate dosing can be achieved by developing methods based on metabolic and phenotypic specifics rather than mere physical measurements.
Guidelines for Calculating Chemotherapy Dose
Example 1: Body Surface Area Method
The Body Surface Area (BSA) method is commonly used to calculate chemo doses. First, determine the BSA using the patient's height and weight. For instance, if using the Mosteller formula: BSA (m^2) = \sqrt{(\text{height (cm)} \times \text{weight (kg)}) / 3600}. Then, multiply the BSA by the drug's dosage prescribed per square meter. If the dosage is 100 mg/m2 and the BSA is 1.8 m2, the dose is 100 \text{ mg/m}^2 \times 1.8 \text{ m}^2 = 180 \text{ mg}.
Example 2: Fixed Dose Calculation
In fixed dose calculations, administer a specific dose, regardless of patient size or BSA. For drugs with a fixed dose protocol, calculate simply by administering the stated dose. Example: If the fixed dose is 200 mg, administer 200 mg.
Example 3: Dosage per Weight
For weight-based dosing, calculate the dose based on the patient’s body weight. Example: If the drug requires 30 mg/kg and the patient weighs 70 kg, the required dose is 30 \text{ mg/kg} \times 70 \text{ kg} = 2100 \text{ mg}.
Example 4: Adjustment for Renal Function
Chemo doses may need adjustment based on renal function, typically measured by creatinine clearance. For a drug where dosage adjustment is necessary, determine the dosage factor from the creatinine clearance level and adjust accordingly. Example: If the base dose is 300 mg and the adjustment factor for a clearance of 50 mL/min is 0.75, then the dose becomes 300 \text{ mg} \times 0.75 = 225 \text{ mg}.
Discover the Power of Sourcetable for All Your Calculation Needs
Intuitive AI-Powered Calculations
Sourcetable revolutionizes data processing with its advanced AI-powered spreadsheet. Designed to handle diverse computation requests, it can effortlessly manage complex calculations across various domains. Whether you're managing financial forecasts, engineering logistics, or educational assignments, Sourcetable simplifies these tasks with precision.
Specialized Applications: Medical Dosage Calculations
For healthcare professionals, calculating correct dosages is crucial. Sourcetable stands out in calculating medical doses, such as how to calculate chemo dose. By simply entering patient data and dosage parameters, the AI analyzes and provides accurate dosage calculations in real-time, ensuring safety and efficacy in patient treatments.
Efficient Learning and Problem Solving
Sourcetable's AI assistant not only performs calculations but also explains them through its chat interface. This feature is invaluable for students and professionals keen to understand the logic behind every computation. It's an effective learning tool that enhances understanding and improves problem-solving skills.
Streamlined for Professional and Educational Use
With Sourcetable, users from various fields can increase productivity and reduce errors in calculations. Its versatility and ease of use make it an excellent tool for educational purposes and professional settings alike, proving that it's more than capable of meeting a wide range of computational needs.
Use Cases for Calculating Chemotherapy Dose
Personalized Chemotherapy Dosing |
By calculating doses based on individual metabolic phenotypes, renal function, and blood counts, healthcare providers can tailor chemotherapy treatments to each patient's unique physiological profile. This approach optimizes efficacy and minimizes toxicity, potentially improving patient outcomes. |
Adjustment for Body Composition |
Advanced body measurement techniques allow for the assessment of body composition and muscle mass, leading to more accurate dose calculations. This is particularly relevant in obese patients, who may have altered drug clearance rates, thereby requiring modified dosing to prevent underdosing and severe toxicities. |
Dose Optimization in Obese Patients |
Obesity impacts chemotherapy dosing by affecting drug clearance and distribution. Using advanced dosing methods that account for body composition can help achieve optimal drug exposure, reducing the risk of severe toxicities like febrile neutropenia and improving overall survival in this population. |
Reduction of Dosing Errors |
By moving away from traditional body surface area (BSA)-based methods to more precise techniques, such as toxicity-adjusting dosing, the frequency of common dosing errors like underdosing or overdosing can be reduced. This ensures that patients receive the most effective therapeutic dose with minimized risk of myelosuppression and other dose-related toxicities. |
Enhancing Efficacy and Survival Rates |
Proper dose calculation methods, especially in testicular cancer and other sensitive conditions, may lead to higher cure rates and improved survival. Adjusting doses based on drug elimination processes and patient-specific factors such as genetic and environmental influences on drug metabolism can significantly enhance treatment efficacy. |
Supporting Clinical Trials |
Accurate dose calculation is crucial in clinical trials to ensure that findings on drug efficacy and safety are reliable. By using individualized dosing strategies, researchers can better understand the pharmacodynamics and pharmacokinetics of chemotherapeutic agents in varied patient populations. |
Frequently Asked Questions
What are the limitations of using body surface area (BSA) to calculate chemotherapy dosage?
BSA-based dosing is criticized for being an inaccurate method as it does not account for individual variations in drug clearance or distribution and elimination of cytotoxic drugs, potentially leading to underdosing or overdosing.
What other methods can be used to calculate chemotherapy dosage besides BSA?
Other methods include adjusting doses based on metabolic phenotype, renal function, and blood counts. Additionally, advanced body measurement techniques and 3D imaging technology may provide more accurate individualized dosing by improving body shape measures.
What is the impact of underdosing in chemotherapy?
Underdosing in chemotherapy may lead to reduced effectiveness, lower cure rates for certain cancers like testis cancer, and decreased survival rates.
How can obesity affect chemotherapy dosing calculations?
Obesity influences chemotherapy dosing by potentially increasing toxicity and mortality. The ASCO has recommended full weight-based dosing in obese patients to counteract these effects.
What measures are recommended to ensure the accuracy of chemotherapy dosing calculations?
Using evidence-based formulas, verifying chemotherapy drug orders for safety, and practicing with case scenarios are recommended measures to ensure accurate chemotherapy dosing calculations.
Conclusion
Calculating the correct chemo dose is crucial for effective treatment and patient safety. Factors such as body surface area (BSA), which can be calculated using the formula BSA = \sqrt{\frac{height(cm) \times weight(kg)}{3600}}, play a significant role in determining the right dosage. Accurate calculations help minimize the risk of underdosing or overdosing, which can lead to severe side effects or reduced efficacy of treatment.
Simplifying Calculations with Sourcetable
Sourcetable, an AI-powered spreadsheet, revolutionizes the way healthcare professionals can manage and perform complex calculations, like chemo dosages. Its intuitive interface and powerful computing capabilities make it easy to apply formulas, analyze data, and verify results. You can even test your calculations on AI-generated data, ensuring accuracy before clinical application.
Experience the benefits of streamlined and efficient calculation processes at app.sourcetable.com/signup, where you can try Sourcetable for free.
Recommended Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.
- how to do dosage calculations
- how to calculate dose per kg body weight
- how to calculate dosage by weight
- is dosage calculations hard
- how to calculate ceftriaxone dose
- how to calculate continuous albuterol dosage
- how to calculate how much oxygen to give a patient
- should you round up or down when calculating lethal dose