Introduction
Calculating fluid restriction in Chronic Kidney Disease (CKD) is crucial for maintaining optimal fluid balance and preventing complications like fluid overload. This balance is essential, as CKD affects the kidneys' ability to regulate fluid in the body. Understanding how to manage fluid intake can significantly improve quality of life and health outcomes for individuals with CKD.
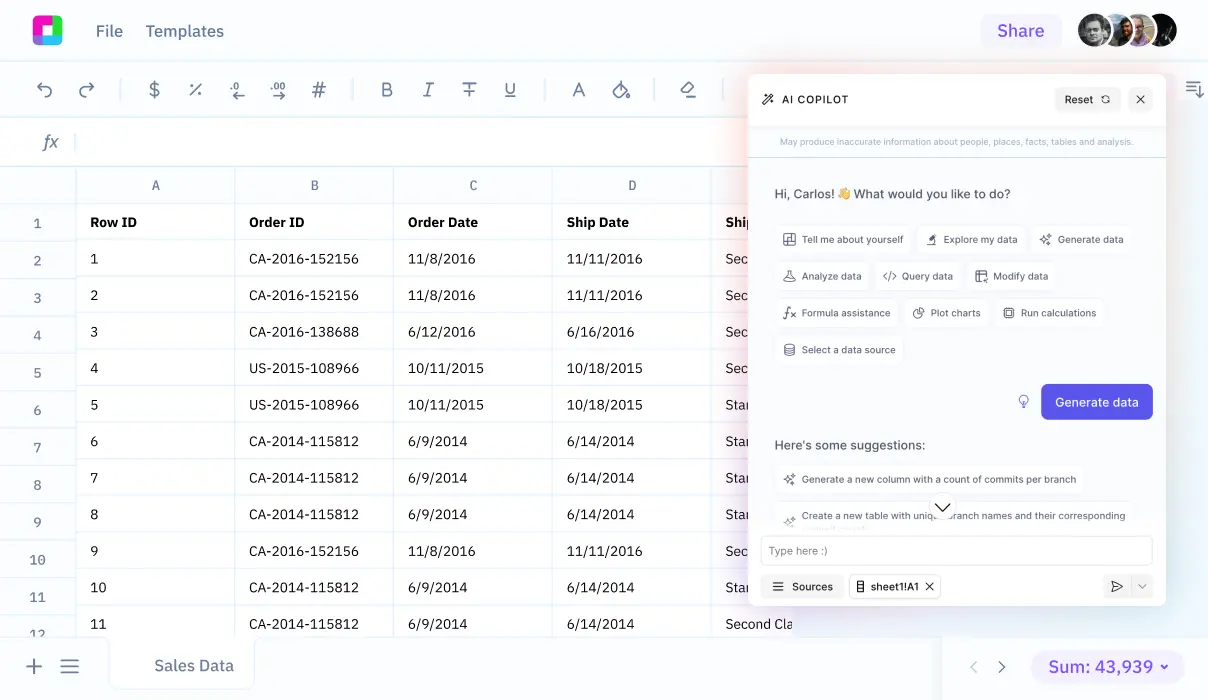
This guide lays out a straightforward method to calculate fluid restrictions tailored for CKD patients. Utilizing clear, actionable steps, it facilitates better management of fluid intake. Further on, we'll reveal how Sourcetable can simplify this process through its AI-powered spreadsheet assistant. Discover how you can effortlessly manage such calculations by signing up at app.sourcetable.com/signup.
See how easy it is to fluid restriction in ckd with Sourcetable
How to Calculate Fluid Restriction in CKD
To calculate fluid restriction in chronic kidney disease (CKD), it is critical to assess kidney function accurately. This measurement determines how well the kidneys can filter and manage fluid balance. Consider the amount of urine produced and the overall filtering capability of the kidneys.
Considerations for Fluid Restriction Calculation
Begin by evaluating the patient's stage of CKD, focusing on stages 4 and 5 for more stringent fluid restrictions. Fluid prescriptions vary depending on kidney function and how effectively the kidneys are filtering waste from the blood.
Method: Calculate fluid intake limits based on the residual kidney function. In patients with minimal urine output and advanced CKD, strict limitations are often necessary.
Special Cases: Dialysis and Transplant Patients
Adjustments need to be made for patients undergoing treatments for end-stage kidney disease. Hemodialysis patients should have a reduced fluid intake to prevent complications such as low blood pressure and heart strain. Conversely, peritoneal dialysis patients may have fewer restrictions, depending mostly on their sodium and sugar consumption, which can affect thirst and fluid balance. Kidney transplant patients, however, typically require increased fluid intake to support kidney function.
When calculating fluid restriction, use these guidelines for each category of treatment and adapt them based on individual patient assessment and the specific type of dialysis they are undergoing.
How to Calculate Fluid Restriction in CKD
Managing fluid intake is crucial for patients with chronic kidney disease (CKD), particularly those in stages 4 and 5 or on hemodialysis. Fluid prescriptions vary based on kidney function and the specifics of the renal failure treatment.
Assessing Kidney Function
Begin by determining the level of kidney function. Physicians typically calculate this based on glomerular filtration rate (GFR). A lower GFR indicates more severe kidney damage, which requires stricter fluid restrictions.
Determining Fluid Prescription
For patients on hemodialysis, it's essential to know their 'dry weight': their body weight minus any excess fluid. Hemodialysis patients should restrict fluid intake to avoid complications like low blood pressure, cramping, and cardiac stress during treatment sessions. This often translates to limiting fluid intake between dialysis treatments.
Fluid Intake for Peritoneal Dialysis Patients
Individuals on peritoneal dialysis may have less stringent restrictions. They should maintain balanced fluid intake while controlling their sodium and sugar consumption to manage thirst and avoid excessive weight gain.
Calculating Specific Fluid Needs
Doctors generally recommend that hemodialysis patients limit fluid intake to 1-1.5 liters per day depending on residual kidney function and fluid status. This calculation often starts from the dry weight, adjusting based on daily weight monitoring, blood pressure levels, and signs of fluid retention such as swelling or shortness of breath.
Kidney transplant patients and those undergoing other forms of treatment such as peritoneal dialysis should consult with their healthcare provider for a tailored fluid intake plan, which is often more lenient but requires careful monitoring of electrolytes and hydration levels.
Examples of Calculating Fluid Restriction in CKD
Example 1: Basic Calculation
For a patient with a urine output of 500 ml/day, calculate the fluid restriction by adding 500 ml to a desirable additional intake, often around 750 ml. Thus, the fluid restriction would be 1250 ml/day.
Example 2: Account for Other Fluid Losses
In cases where a patient experiences additional fluid losses through perspiration, vomiting, or diarrhea, adjust the basic calculation. If a patient loses an extra 300 ml/day through perspiration, the fluid restriction becomes 1550 ml/day (adding the extra loss to the basic calculation).
Example 3: Adjustments for Hemodialysis
Patients undergoing hemodialysis might have different restrictions. Assume the standard calculation gives 1000 ml/day. After dialysis, which removes approximately 2000 ml of fluid, the patient may be allowed a higher fluid intake before the next session, adjusted according to the frequency of dialysis.
Example 4: Incorporating Clinical Adjustments
Clinical adjustments may be necessary based on a patient's overall health and other factors like heart failure or edema. If a patient’s condition suggests a lower tolerance for fluid, the medical team might reduce the fluid intake limit by 200-300 ml from the standard calculation to prevent fluid overload.
Example 5: Progressive Adjustments
Progressive adjustments are critical as CKD advances. For a hypothetical fluid restriction initially set at 1500 ml/day, a progression in CKD stage might warrant a decrement by 250 ml, bringing the restriction to 1250 ml/day to decrease the burden on kidney function.
Unlock the Power of AI with Sourcetable
Efficiency in Complex Calculations
Calculate anything quickly and accurately with Sourcetable's AI-powered spreadsheet. Simplify complex calculations like how to calculate fluid restriction in CKD without the hassle of manual errors or complicated formula setup. Sourcetable streamlines the process, from input to solution.
Tailored Explanations
Benefit from real-time explanations as Sourcetable’s chat interface details the steps behind each calculation. Understand not just the fluid restriction result, but also the methodology, enhancing both learning and application.
Optimal Tool for Education and Professional Tasks
Whether you're a student, a healthcare professional, or someone keen on accurate calculations, Sourcetable serves all. It’s an invaluable tool for academic study, professional work, and everyday problem-solving.
Use Cases for Calculating Fluid Restriction in Chronic Kidney Disease (CKD)
1. Enhancing Patient Safety |
Knowing how to calculate fluid restriction helps prevent fluid overload, reducing the risk of swelling, shortness of breath, and organ damage. This ensures patient safety, especially during late-stage CKD or when on hemodialysis. |
2. Improving Treatment Compliance |
Patients on hemodialysis can use their dry weight and daily weight changes to adhere to their fluid restriction guidelines, improving treatment compliance and reducing complications. |
3. Individualized Patient Care |
Fluid needs vary with the degree of kidney function and the type of kidney disease treatment. Calculating precise fluid restrictions enables healthcare providers to tailor treatments to individual patient needs, enhancing overall care. |
4. Dietary Management |
Understanding fluid calculation aids in dietary management. Patients learn the benefits of low salt intake to control thirst and fluid intake, promoting better health outcomes. |
5. Medication Effectiveness |
Proper fluid calculation allows for more effective use of medications such as diuretics, which help maintain fluid balance, prevent fluid retention, and avoid medication-induced complications. |
6. Prevention of Hospitalization |
Correct fluid restriction calculation aids in preventing conditions like heart failure and severe edema, which could lead to hospitalization, by managing fluid overload effectively in CKD patients. |
7. Facilitating Recovery Post-Transplant |
Knowing how to adjust fluid intake post-kidney transplant is crucial. Increased fluid intake is often necessary, and proper calculations ensure the new kidney functions optimally. |
8. Enhancing Quality of Life |
Accurate fluid restriction calculations contribute to a better quality of life by avoiding discomfort and complications associated with improper fluid intake in CKD patients. |
Frequently Asked Questions
How is fluid restriction calculated for patients with chronic kidney disease?
Fluid restriction in chronic kidney disease (CKD) is calculated based on the individual's kidney function, amount of residual kidney function, and whether they are undergoing treatments like hemodialysis. Healthcare providers also consider symptoms of fluid overload and daily urine output to tailor fluid prescriptions.
What factors influence fluid prescriptions in CKD patients?
Factors influencing fluid prescriptions include the stage of kidney disease, effectiveness of the kidneys in balancing fluids and removing waste, and whether the patient is undergoing treatment like hemodialysis or has had a kidney transplant. Fluid restrictions may also be adjusted based on the presence of symptoms like swelling or high blood pressure.
Why do hemodialysis patients need to restrict fluids?
Hemodialysis patients need to restrict fluids to prevent fluid overload, which their kidneys can no longer manage effectively. Excess fluids can lead to serious health issues such as swelling, high blood pressure, heart failure, and complications affecting the lungs.
How can hemodialysis patients manage their fluid intake?
Hemodialysis patients can manage their fluid intake by monitoring their dry weight, reducing salt intake to lessen thirst, checking their blood pressure and daily weight, following medication instructions carefully, and adopting new habits like drinking smaller amounts of water throughout the day.
What should patients do if they are unsure about their fluid intake restrictions?
Patients unsure about their fluid intake restrictions should consult with their healthcare team or a kidney dietitian. These professionals can provide personalized guidance based on the patient’s specific condition, kidney function, and treatment plan.
Conclusion
Calculating fluid restriction in chronic kidney disease (CKD) is crucial for managing symptoms and preventing further complications. The formula fluid intake = urine output + 500 ml helps determine the daily fluid intake. However, individual factors such as stage of CKD, body weight, and other health conditions might affect this calculation.
The Role of Sourcetable in Calculations
Sourcetable simplifies the process of calculating fluid restrictions in CKD. As an AI-powered spreadsheet, it facilitates efficient and accurate calculations, allowing users to focus more on clinical decision-making rather than the intricacies of manual computation. Try your own calculations using AI-generated data to simulate different scenarios and optimize patient care strategies.
Experience the ease of Sourcetable by signing up for free at app.sourcetable.com/signup.
Recommended Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.