Turn Claims Data Into Strategic Advantage
Insurance claims data analysis transforms raw claim information into actionable intelligence that reduces losses, accelerates processing, and improves underwriting accuracy. From detecting fraudulent patterns to predicting claim severity, sophisticated analysis of claims data enables insurers to make better decisions faster while controlling costs.
Traditional claims analysis relies on manual review and basic statistical summaries—average claim amounts, frequency by category, simple trend tracking. Modern analytics goes deeper, uncovering subtle patterns that indicate fraud, identifying risk factors that predict future claims, and optimizing operational processes to reduce expenses.
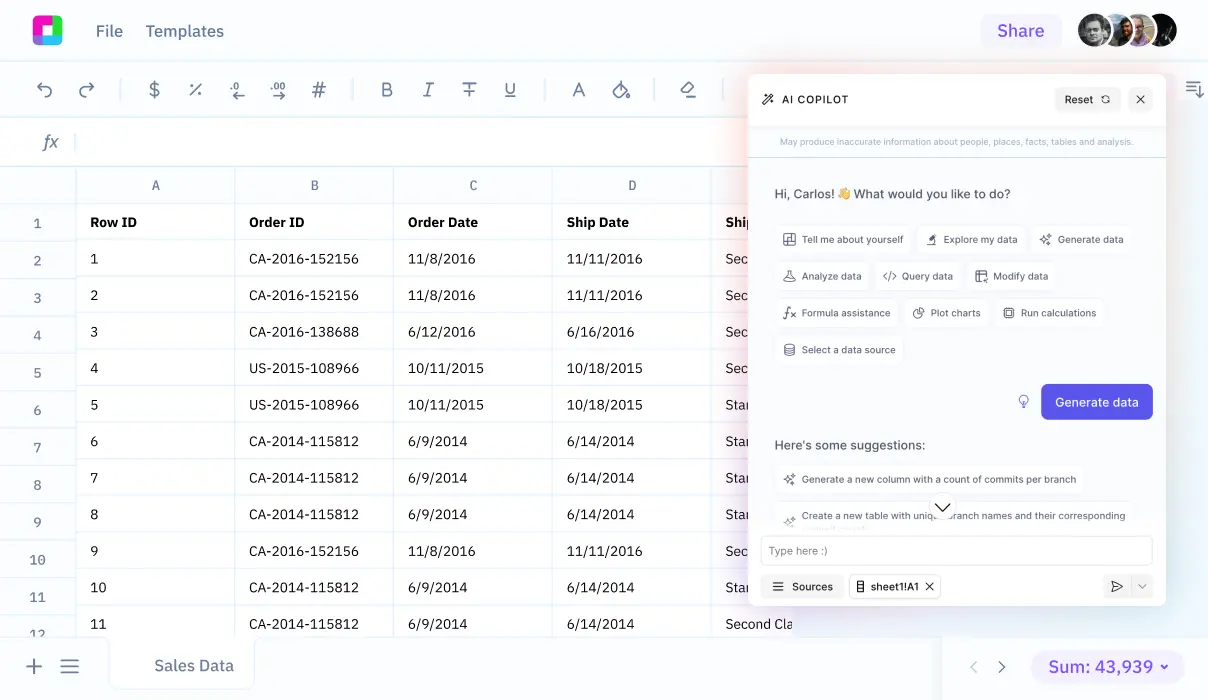
Sourcetable brings advanced claims analytics to insurance professionals without requiring data science expertise. Import claims data from core systems, use natural language to ask analytical questions, and receive insights that drive measurable improvements in loss ratios, fraud detection rates, and claim processing efficiency.
Why Insurance Claims Analysis Matters
Insurance Claims Analysis Matters
Detect Fraudulent Claims
Identify fraud patterns through anomaly detection, network analysis, and historical comparison. Flag suspicious claims based on behavioral patterns, documentation inconsistencies, or unusual claim characteristics. Early fraud detection prevents costly payouts and reduces investigation expenses.
Optimize Claims Processing
Analyze processing workflows to identify bottlenecks, prioritize high-value claims, and automate routine decisions. Reduce cycle time, improve customer satisfaction, and decrease operational costs. Track adjuster performance and workload balance for resource optimization.
Improve Underwriting Decisions
Use historical claims data to refine risk models, adjust pricing, and identify profitable market segments. Understand which applicant characteristics correlate with higher or lower loss ratios. Make data-driven decisions on coverage terms and premium pricing.
Predict Claim Severity
Forecast expected claim costs at filing time using predictive modeling. Allocate appropriate reserves, prioritize adjuster assignment, and intervene early on high-severity claims to minimize losses. Improve reserve accuracy and reduce development volatility.
Insurance Claims Analysis Applications
Real-world applications and use cases
Fraud Detection and Investigation
Analyze claim patterns to identify fraudulent submissions. Flag claims with characteristics common to known fraud—unusual damage patterns, provider networks, claim timing, or claimant history. Prioritize special investigation unit (SIU) resources on highest-risk claims.
Subrogation Opportunity Identification
Identify claims with subrogation potential by analyzing fault patterns, third-party involvement, and claim characteristics. Quantify potential recovery amounts and prioritize subrogation efforts. Track recovery rates and optimize subrogation strategy.
Medical Claims Cost Containment
Analyze healthcare utilization patterns, treatment costs, and provider behavior in medical claims. Identify over-utilization, unnecessary treatments, or billing irregularities. Implement utilization review and case management for high-cost claims.
Property Claims Damage Assessment
Analyze property damage claims to predict repair costs, identify appraisal issues, and detect estimate manipulation. Compare actual vs. estimated costs to improve appraisal accuracy and identify contractors with consistent overruns.
Insurance Claims Analysis Workflow in Sourcetable
Step-by-step workflow guide
Import Claims Data
Connect to claims management systems, policy administration platforms, or upload claims exports. Sourcetable handles data from all major insurance systems and automatically structures claim details, dates, amounts, and statuses for analysis.
Data Quality and Enrichment
Validate data completeness, clean inconsistencies, and enrich claims with external data (weather, demographics, economic indicators). AI flags data quality issues and suggests resolution strategies.
Exploratory Analysis
Examine claim distributions, trends over time, and patterns by category, geography, or policy type. Identify anomalies, seasonal effects, and emerging trends. Generate summary statistics and visualizations to understand your claims portfolio.
Fraud Detection
Apply anomaly detection algorithms to flag potentially fraudulent claims. Analyze network connections between claimants, providers, and attorneys. Score claims by fraud risk using machine learning models trained on historical fraud cases.
Common Fraud Indicators in Claims Data
Claimant Red Flags
Multiple claims within short timeframes, especially across different insurers. Claim history showing pattern of losses just before policy cancellation. Lack of corroborating evidence or inconsistent statements. New policy with immediate claim. Uncooperative with investigation or overly familiar with claims process.
Provider and Vendor Red Flags
Unusually high volume of claims from specific providers, repair shops, or medical facilities. Charges significantly above market rates. Consistent patterns of specific diagnoses or procedures. Networks of related providers, attorneys, and claimants appearing together across multiple claims.
Claim Characteristic Red Flags
Losses occurring shortly after policy changes that increase coverage. Suspicious timing—claims filed just before weekends, holidays, or policy expiration. Damage inconsistent with reported cause of loss. Lack of police reports or witness statements when expected. Padded or inflated estimates.
Network Analysis
Fraud rings often involve repeated connections between claimants, providers, attorneys, and witnesses. Network analysis reveals these relationships, identifying clusters of potentially fraudulent activity. Track social connections, shared addresses, phone numbers, or bank accounts across claims.
Anomaly Detection
Statistical outliers deserve investigation. Claims with characteristics significantly different from typical patterns—unusually high amounts, uncommon loss types, atypical claimant demographics for the policy type, or geographical anomalies. Machine learning excels at identifying subtle anomalies human reviewers miss.
Essential Insurance Claims Metrics
Loss Ratio
Incurred losses divided by earned premiums, expressed as a percentage. The fundamental profitability metric for insurance operations. Track by line of business, geography, policy type, and time period. Target loss ratios vary by line but typically range from 60-75% for profitable operations.
Claim Frequency and Severity
Frequency measures claims per exposure unit (e.g., claims per 100 insured vehicles). Severity measures average cost per claim. Both drive overall losses, but respond to different interventions. Frequency reduction targets loss prevention; severity reduction focuses on claim management.
Cycle Time
Days from loss date or report date to claim closure. Fast cycle time improves customer satisfaction and reduces administrative costs. Track separately for different claim types as complexity varies. Monitor for process bottlenecks that delay settlement.
Closure Rate
Percentage of claims closed within specific timeframes (30, 60, 90 days). Indicates processing efficiency and adjuster productivity. Low closure rates suggest capacity issues, complex claims mix, or process problems requiring attention.
Reserve Adequacy
Compare initial case reserves to final settlement amounts. Consistent under-reserving indicates reserve setting models need recalibration. Over-reserving ties up excess capital. Track reserve development patterns to improve accuracy and reduce volatility.
Litigation Rate
Percentage of claims involving attorney representation or litigation. Litigated claims cost 2-5x more than similar non-litigated claims. Identify factors driving litigation and implement early intervention strategies to reduce litigation rates.
Frequently Asked Questions
What data do I need for effective insurance claims analysis?
Core data includes claim details (loss date, report date, type, status), amounts (reserves, payments, expenses), policy information (coverage, limits, premium), and outcome data (settlement, subrogation, litigation). Enhanced analysis benefits from adjuster notes, medical records, repair estimates, and external data like weather or economic conditions. Sourcetable works with data exports from any claims system.
How accurate is AI-based fraud detection compared to manual investigation?
AI fraud detection identifies 2-3x more potential fraud cases than traditional rule-based approaches, with 30-50% reduction in false positives. However, AI flags suspicious claims for investigation—it doesn't replace human investigators. The combination of AI screening plus human investigation is most effective, allowing SIU resources to focus on highest-risk cases.
Can I analyze claims data across multiple lines of business together?
Yes, multi-line analysis reveals cross-selling opportunities, identifies customers with excessive claims across multiple policies, and enables enterprise-wide loss trends analysis. However, maintain line-specific models for pricing and reserving since claim characteristics differ significantly between auto, property, workers compensation, and other lines.
How do I ensure claims analysis complies with privacy regulations?
Insurance claims contain sensitive personal information subject to privacy laws. Sourcetable implements role-based access controls, data encryption, and audit logging. For analysis, use de-identified data when possible. Implement data retention policies aligned with regulatory requirements. Document analytical procedures for regulatory examinations.
What's the typical ROI from claims analytics initiatives?
Well-executed claims analytics programs typically deliver 3-5% improvement in loss ratios within 12-18 months through fraud detection, subrogation recovery, and claims management optimization. Additional benefits include 15-30% reduction in claim processing costs, improved reserve accuracy, and better underwriting performance. ROI depends on claim volume and current analytics maturity.
How often should I refresh claims analysis models?
Predictive models for fraud detection, severity, or litigation should be retrained at least annually as claim patterns evolve. Operational dashboards need daily or weekly updates to track current performance. Strategic analyses (market trends, loss cost studies) typically update quarterly. Set up automated data pipelines so fresh data flows continuously without manual intervention.
Related Analysis Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us