Introduction
Understanding how to calculate total parenteral nutrition (TPN) is crucial for healthcare professionals managing the nutritional needs of patients who cannot eat by mouth. Accurate TPN calculations support patient recovery and prevent complications associated with nutrient imbalances. This guide provides a step-by-step approach to calculating macronutrients and micronutrients, fluid volumes, and infusion rates required for effective TPN therapy.
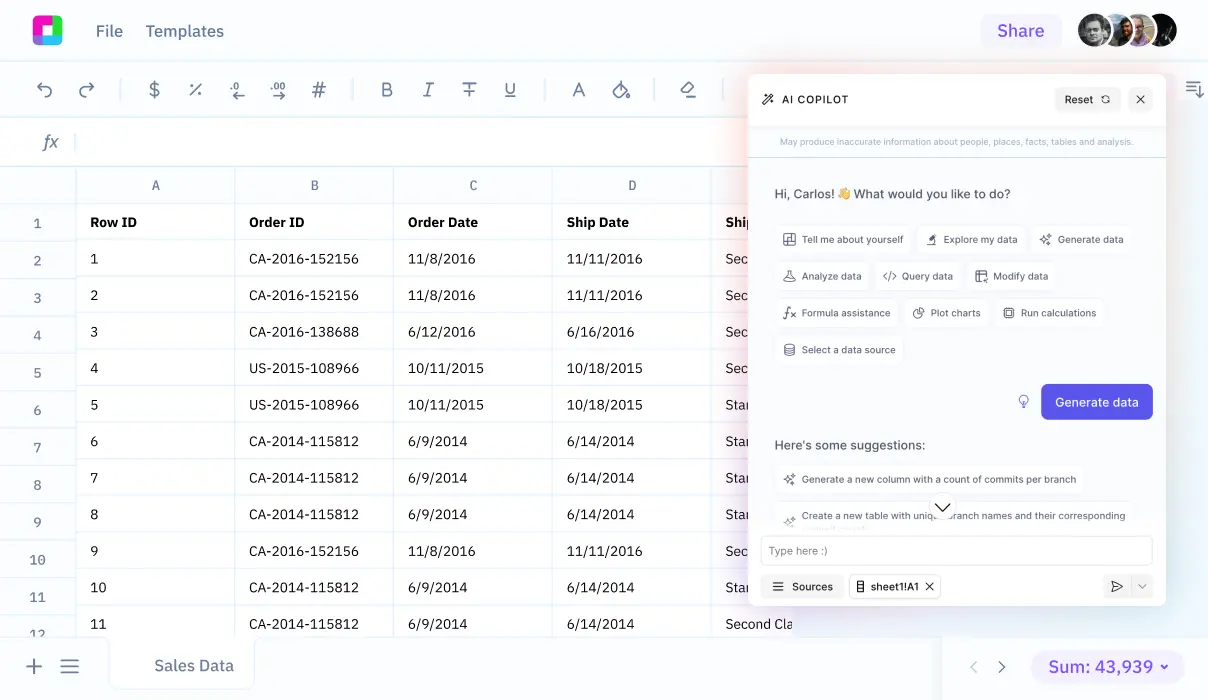
We'll also explore how Sourcetable can simplify this process. Sourcetable offers an AI-powered spreadsheet assistant that enhances efficiency and accuracy in medical calculations. Try it by visiting app.sourcetable.com/signup.
See how easy it is to total parenteral nutrition (tpn) with Sourcetable
How to Calculate TPN: A Step-by-Step Guide
Determining Fluid Requirements
To initiate TPN calculation, estimate the patient's fluid needs using the Holliday-Segar Method. This method calculates necessary fluid based on body weight.
Estimating Caloric Needs
Use the Harris Benedict Equation to predict baseline caloric requirements. For more precise measurements, especially in critical care, a Metabolic Cart Study is advisable. Adjust caloric intake based on metabolic status: use 25-30 kcal/kg/day for normometabolic patients, 20-25 kcal/kg/day for hypometabolic patients, and 30-35 kcal/kg/day for hypermetabolic patients.
Calculating Macronutrient Needs
TPN requires careful calculation of macronutrients—proteins, fats, and carbohydrates. For proteins, dosing ranges from 0.8g/kg (maintenance) to 2-3g/kg (conditions like burns or major injuries). Carbohydrates are calculated based on a caloric density of 3.4 kcal/g, and fats are calculated at 9 kcal/g. These estimates should be tailored while maintaining overall caloric goals.
Micronutrient and Electrolyte Estimation
Key micronutrients include magnesium (12-16 mEq/L), calcium (10 mEq/L), and phosphorus (25 mMol/L). Adjust micronutrient dosing as needed. For example, omit manganese and copper if liver function tests exceed normal limits, as these can lead to manganese toxicity or copper deficiency respectively.
Finalizing the TPN Formula
After calculating individual component needs, cross-multiplications are used to determine precise dextrose concentrations and lipid volumes. This customization ensures that metabolic demands are met without exceeding fluid capacity.
Rate of Infusion
The final step involves setting up the rate of infusion to meet calculated nutritional goals while ensuring patient safety and comfort.
By meticulously following these steps, healthcare providers can precisely compose a TPN regimen tailored to individual patient needs.
How to Calculate TPN
Evaluating the Need for TPN
Start by assessing whether the patient requires total parenteral nutrition (TPN). This involves considering both the necessity based on their medical condition and any contraindications for TPN use.
Calculating Fluid Needs
Determine the patient's fluid requirements using the Holliday-Segar method. This calculation considers the patient’s weight, ensuring hydration levels are maintained without exacerbating any existing conditions.
Calculating Macronutrient Needs
Estimate macronutrient needs based on the patient’s metabolic demands, which can be determined using the Harris Benedict equation or a metabolic cart. Protein needs vary by the patient's condition, ranging from 0.8 to 3 g/kg depending on stress levels and metabolic demands. Use empirical dosing for macronutrients while maintaining the desired daily calorie intake.
Specific Macronutrient Calculations
Calculate protein, fat, and carbohydrate needs individually:
- Protein: Adjust the amount from 0.8 g/kg to 3 g/kg based on the patient’s condition and metabolic stress.
- Fat: Determine fat needs in correlation with the calculated fluid volume since total calories include both fat and carbohydrates.
- Carbohydrates: Calculate after setting protein and fat needs, ensuring they complement the remaining caloric requirements.
Calculating Micronutrient Needs
Assess the necessity for and appropriate dosages of vitamins and minerals, which are crucial for preventing deficiencies during TPN therapy.
Preparing and Administering TPN
Follow strict sterility protocols to mix and administer TPN. Use a central line dedicated to TPN to minimize infection risks. Always monitor the patient’s response to the therapy closely, adjusting the nutrient composition as necessary.
Monitoring and Adjusting
Regularly adjust TPN formulations based on ongoing assessments of the patient's metabolic needs, lab results, and overall health status. Consult healthcare professionals immediately if any unusual events occur during the infusion process.
Examples of Calculating Total Parenteral Nutrition (TPN)
Example 1: Basic TPN Calculation
Determine the daily caloric needs for a 70 kg adult with a basal energy expenditure (BEE) of 25 kcal/kg/day. The calculation is: 70 kg x 25 kcal/kg/day = 1750 kcal/day. Adjust the caloric intake based on patient's condition and activity level.
Example 2: Macronutrient Calculation in TPN
For a patient requiring a higher protein intake due to recovery from surgery, calculate protein needs at 1.5 g/kg/day. For a 70 kg patient, the calculation is: 70 kg x 1.5 g/kg/day = 105 g of protein/day. Ensure compatibility of amino acid composition in TPN solution.
Example 3: Electrolyte Addition
Calculate potassium needs for a patient. Standard recommendation is 1 mEq/kg/day. For a 70 kg patient: 70 kg x 1 mEq/kg/day = 70 mEq/day. Monitor serum electrolyte levels to adjust the dosage as necessary.
Example 4: Fluid Volume Calculation
Determine total fluid volume for TPN. A guideline is 30 mL/kg/day for an adult. For a patient weighing 70 kg, the necessary fluid volume is: 70 kg x 30 mL/kg/day = 2100 mL/day. Adjust based on hydration status and renal function.
Example 5: Lipid Component Calculation
Calculate lipids as part of the total calorie intake at 30%. If total caloric requirement is 1750 kcal/day, calculate lipid needs: 0.30 x 1750 kcal = 525 kcal from lipids/day, translating to about 58 g of lipids/day (since 1 g of lipid provides approximately 9 kcal).
Master Complex Calculations with Sourcetable
Sourcetable, an AI-powered spreadsheet tool, revolutionizes the way we approach complex calculations. Tailored for both educational and professional use, it simplifies computational tasks by incorporating an intelligent AI assistant.
How to Calculate TPN with Sourcetable
Total Parenteral Nutrition (TPN) calculations are essential in medical settings, determining the precise nutritional needs for patients who cannot eat by mouth. Sourcetable facilitates these calculations by allowing users to input variables such as patient weight, desired calories, and macronutrient ratios. The AI assistant processes these inputs and computes the necessary formulation with accuracy.
The tool displays results directly in a user-friendly spreadsheet and provides step-by-step explanations through its chat interface. This dual-display feature ensures that users not only receive the answers they need but also understand the computation process. Such features make Sourcetable ideal for healthcare professionals and students in medical fields.
Incorporating Sourcetable into your study or work routine enhances productivity and ensures high accuracy in critical calculations like TPN. The innovative AI assistant supports learning, making complex calculations understandable and accessible to everyone.
Use Cases for Calculating TPN
Managing Patients with Short Gut Syndrome |
Calculating TPN allows clinicians to tailor macronutrient and fluid requirements for patients with short gut syndrome, ensuring these patients receive adequate nutrition intravenously when oral intake is not possible. |
Prevention of Refeeding Syndrome in At-Risk Patients |
Knowledge of TPN calculation helps prevent refeeding syndrome by adjusting the rate and composition of nutrients, especially important in patients with sudden nutritional replenishment after a period of malnourishment or starvation. |
Support for Patients with Multiple Wounds |
Accurate TPN calculations enable the provision of sufficient protein and calories to support wound healing, optimizing recovery in patients with multiple or complex wound injuries. |
Treatment of Patients with Liver Disease |
Calculating TPN for liver disease patients involves adjusting macronutrient ratios to manage protein intake and reduce the risk of complications like hepatic encephalopathy. |
Addressing Nutritional Needs in Hypermetabolic States |
For patients in hypermetabolic states, such as those with severe burns or infections, TPN calculations are critical in providing increased caloric intake using the guideline of 30-35 kcal/kg/day to meet heightened energy demands. |
Management of Glucose Metabolism Issues |
For patients experiencing difficulties with glucose metabolism, TPN calculation assists in crafting a balanced infusion plan that maintains stable blood glucose levels, utilizing adjusted dextrose and insulin dosages. |
Frequently Asked Questions
How do you calculate fluid requirements for TPN?
To calculate fluid requirements for TPN, use the Holliday-Segar Method. For example, a 50kg patient would typically require 2100mL/day.
How do you determine caloric requirements for TPN?
Caloric requirements for TPN can be determined using the Harris Benedict Equation or by using weight-based caloric needs depending on the patient's metabolic state. For instance, calculation methods vary from using actual body weight in obese patients (11-14kcal/kg/day) to considering ideal body weight in patients with a BMI>50 (22-25kcal/kg/day).
What is the recommended protein intake when calculating TPN?
Protein intake recommendations vary based on BMI and patient condition. Generally, protein needs are estimated using 1.2 to 2 g/kg for a BMI <30 kg/m2 and 2 g/kg for BMI >30 kg/m2. These needs can be adjusted based on wound healing and stress levels.
How should fats and carbohydrates be calculated in TPN?
Fat needs are estimated by giving 30-40% of total calories from fat. Carbohydrate needs should make up the remaining caloric requirement after accounting for protein and fat calories.
What factors should be considered when calculating TPN?
When calculating TPN, consider the patient's fluid requirements, metabolic needs, wound healing needs, and specific conditions like refeeding syndrome, liver function and various nutritional deficiencies (e.g., manganese, copper). TPN requirements may also be influenced by specific medical conditions such as patients with short gut syndrome or those undergoing continuous renal replacement therapy.
Conclusion
Mastering the process of how to calculate TPN is essential for ensuring accurate nutrient delivery in clinical settings. This involves calculating macronutrient components, electrolytes, and fluid requirements, which requires precision and attention to detail.
Simplifying Calculations with Sourcetable
Sourcetable, an AI-powered spreadsheet, streamlines these complex calculations. By handling computations efficiently, it allows health professionals to focus on patient care rather than manual calculations. Sourcetable also provides the option to use AI-generated data for testing and improving your calculation skills.
To experience the ease of calculating TPN and other critical formulas, you can try Sourcetable for free at app.sourcetable.com/signup.
Recommended Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.