Introduction
Calculating a heparin drip accurately is crucial for ensuring patient safety and effective treatment. Heparin, a common anticoagulant used to prevent and treat blood clots, requires careful dosage based on the patient's specific health parameters. This webpage guides healthcare providers through the essentials of how to calculate a heparin drip, focusing on the formula, patient weight, and aPTT levels.
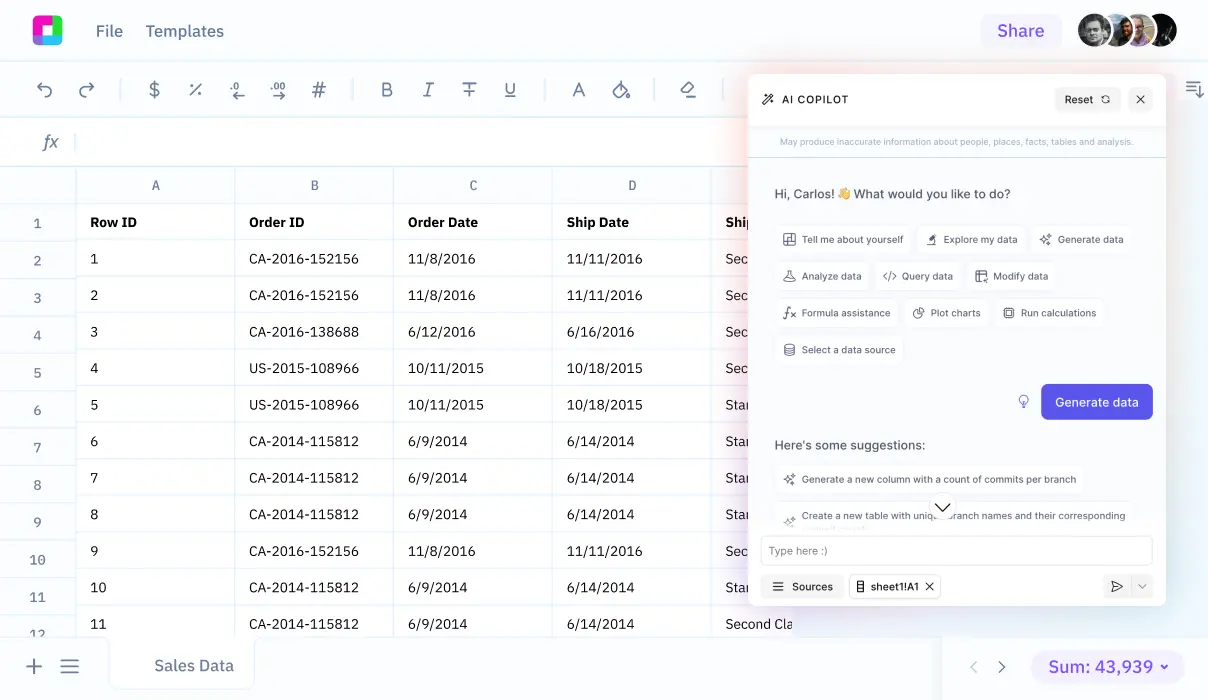
With technological advancements, tools like Sourcetable can streamline complex calculations. We'll delve into how Sourcetable's AI-powered spreadsheet assistant aids in this process, making calculations more efficient and reducing the chance of errors. Experience it firsthand by signing up at app.sourcetable.com/signup.
See how easy it is to heparin drip dosage with Sourcetable
How to Calculate Heparin Drip
Understanding Heparin Drip Calculations
To ensure safe and effective dosage, follow a multi-step process for calculating heparin drip. Start by determining the overall units per hour needed, using the formula units/hour = units × weight in kg/hour. Next, compute the infusion rate: rate of infusion = (total units in IV bag/units per hour) × ml/hour = X ml/hr.
Tools for Accurate Dosage Calculation
The AIC (Automated Impella Controller) and the Systemic IV Heparin Rate Calculator in the Abiomed Clinical Care App are essential tools. The AIC provides details about the heparin delivered through the purge fluid, as seen on its Infusion History screen. This screen assists by displaying an hourly breakdown of fluid and heparin administered to the patient.
Calculating Heparin with Impella
For patients supported with Impella devices, calculate the total heparin rate by accounting for both the systemic drip and the heparin purge fluid. Subtract the heparin amount delivered by the Impella, shown on the AIC, from the total heparin rate as recommended by the hospital protocol or pharmacy.
Dimensional Analysis and Rounding
Utilize dimensional analysis for solving the heparin drip calculations. Always round your final answer based on your facility’s rules, typically to the nearest tenth.
Accessibility of Calculators
The Systemic IV Heparin Rate Calculator supports healthcare professionals by being accessible in various clinical settings, including pre- and post-procedure environments such as the cath lab, ICU, OR, or while in transport.
Calculating Heparin Drip Dosage
Understanding how to calculate heparin drip dosage is crucial for ensuring effective anticoagulation therapy in patients needing continuous intravenous administration. The process involves a combination of hospital protocols and specific calculations to determine the accurate dosage.
Step-by-Step Guide to Heparin Drip Calculation
Begin by determining the total heparin rate required, which includes heparin in both the systemic drip and any device-specific introduction, such as the purge fluid in an Impella device. The AIC’s Infusion History screen can be consulted to assess the heparin given via Impella.
To calculate the systemic IV heparin rate, first use the formula Impella\ delivered\ heparin\ rate = (Heparin\ concentration\ in\ purge\ fluid\ (U/mL)) \times (Infusion\ rate\ (mL/hr)). Then, subtract the Impella delivered rate from the total prescribed heparin rate, aligning with the recommendation from hospital protocols or pharmacy.
After determining the units per hour based on the patient’s weight and prescribed heparin dosage per kg, calculate the total units in an IV bag using Total\ Units\ in\ the\ IV\ bag = Units/hour \times Total\ Volume\ in\ ml. Divide this by the units per hour and multiply by the volume in ml to find the infusion rate in ml per hour. Always round calculations to the nearest tenth to maintain dosage precision.
To find the infusion rate in ml per hour, solve the equation X = \frac{Total\ Units\ in\ IV\ bag}{Units/hour \times Total\ Volume\ in\ ml}, where X represents the heparin infusion rate.
Accurate calculation and consistent monitoring are essential components in managing heparin therapy, ensuring both efficacy and safety in anticoagulation management.
Calculating Heparin Drip: Practical Examples
Example 1: Standard Initiation Protocol
Initiate a heparin drip by calculating the total dose required based on the patient's weight. If a patient weighs 70 kg and the standard dosage is 18 units/kg/hr, the infusion rate would be 70 kg × 18 units/kg/hr = 1260 units/hr. Starting with a bolus dose, often 80 units/kg, calculate as 70 kg × 80 units/kg = 5600 units initial bolus. Use an infusion pump to deliver this calculated rate accurately.
Example 2: Adjustment According to aPTT
Adjust the heparin dosage based on activated partial thromboplastin time (aPTT) results. If the target aPTT is 60 seconds and the observed aPTT is 45 seconds, increase the rate by 2 units/kg/hr. For a 60 kg patient, the new rate is (60 kg × 2 units/kg/hr) + existing rate. Continue to monitor and adjust as necessary.
Example 3: Renal Impairment Adjustment
In patients with renal impairment, decrease the heparin rate due to reduced clearance. If the creatinine clearance is 30 mL/min, reduce the rate by 30%. For an initial rate of 1000 units/hr, the adjusted rate would be 1000 units/hr × 0.70 = 700 units/hr. Monitor renal function and aPTT closely.
Example 4: Transition to Oral Anticoagulants
When transitioning from heparin to an oral anticoagulant like warfarin, overlap heparin therapy with warfarin until the INR is therapeutic for 24 hours. If INR is 2.0 and the goal is 2.5, continue heparin at the current rate and adjust warfarin dose as per INR response. Discontinue heparin once INR is stable and within the target range.
Example 5: Weight-Based Titration in Obesity
For obese patients, titrate heparin based on adjusted body weight. If actual body weight is 120 kg and the dosing weight is 90 kg (using a dosing cap), calculate the infusion rate at 15 units/kg/hr as 90 kg × 15 units/kg/hr = 1350 units/hr. Regularly reassess weight and adjust the dosage accordingly.
Discover the Power of Sourcetable for All Your Calculation Needs
Sourcetable redefines efficiency with its AI-powered spreadsheet capabilities. Tailored to handle any computation, from simple arithmetic to complex algorithms, this tool is indispensable for academic, professional, and personal projects.
Seamlessly Calculate Heparin Drips
Understanding how to calculate a heparin drip is crucial in medical settings. Sourcetable simplifies this with precision and real-time explanations. Input your variables, and let the AI assistant do the rest, displaying both the answer and the step-by-step process in an easy-to-understand format.
Sourcetable is not just a calculator but a comprehensive learning tool. Whether you're preparing for exams or need accurate calculations at work, Sourcetable provides the support you need to succeed. Embrace the future of calculations with Sourcetable at your side.
Use Cases for Calculating Heparin Drip
Handling Acute Cardiovascular Conditions |
For patients experiencing a heart attack or undergoing heart surgery, angioplasty, or stent placement, calculating the heparin drip accurately ensures rapid and effective management of potential thrombotic complications. |
Management of Venous Thromboembolism (VTE) |
In cases like deep vein thrombosis or pulmonary embolism, proper calculation of heparin drip based on Units/hour = (Total Units in IV bag) / (Total Volume in mL) X (mL/hour) supports immediate and precise anticoagulation therapy, promoting clot resolution and preventing further embolic events. |
Prevention of Clotting in Extracorporeal Circuits |
During dialysis or in patients with mechanical heart valves, accurate heparin dosing prevents the formation of clots in the machine or around the artificial valve, assuring the smooth functioning of the mechanical processes and patient safety. |
Treatment Adjustments Based on Patient Response |
Because heparin's effectiveness and safety require monitoring via blood tests, knowing how to adjust the drip rate based on patient's response is critical. Adjustments are calculated by X = (Total Units in IV bag) / (500 mL), ensuring the dose remains therapeutic but not excessive. |
Effective Management of Pregnancy-Related Complications |
In pregnant women experiencing complications related to clotting, precise heparin drip calculations help manage the condition without harming the fetus, providing critical care in a sensitive patient population. |
Emergent Treatment for Stroke and Limb Ischemia |
Dosing calculations in the acute management of stroke and arterial blockages in limbs ensure timely and sufficient anticoagulation to mitigate the risk of further ischemic damage. |
Frequently Asked Questions
How do you calculate the total heparin rate for a patient with an Impella device?
To calculate the total heparin rate for a patient with an Impella device, include the heparin delivered by both the systemic drip and the purge fluid. You can find the heparin delivered by the Impella on the Infusion History screen of the AIC. The total heparin rate is calculated by subtracting the heparin delivered by the Impella from the total rate recommended by the hospital protocol or pharmacy.
How do you determine the infusion rate for a heparin drip?
To determine the infusion rate for a heparin drip, first calculate the units of heparin per hour by multiplying the units per kg per hour by the patient's weight in kg. Use this result to solve the formula: Total Units in IV bag / Total Volume in ml = Units/hour (solve for X, where X is the infusion rate in ml/hour).
How do you adjust a heparin drip based on aPTT levels?
To adjust a heparin drip based on aPTT levels, increase the drip rate if the patient’s PTT is too low, or decrease it if the PTT is too high. You may also need to administer a bolus if the PTT is too low or an additional drip if the PTT is too high. Always recheck the PTT after making any changes.
How is the patient's weight used in calculating heparin drip?
The patient's weight is critical in calculating heparin drip as it is used to determine the total units of heparin per hour. This is done by multiplying the prescribed units of heparin per kg per hour by the patient’s weight in kilograms.
Conclusion
Mastering the calculation of a heparin drip is crucial for effective patient care. Understanding and applying the correct dosages through formulas like dosage = (desired dose × weight × 60) / concentration is essential. Calculating these dosages correctly ensures safety and efficacy in anticoagulant therapy.
Enhance Calculations with Sourcetable
Sourcetable, an AI-powered spreadsheet platform, radically simplifies the execution of complex calculations required for healthcare protocols such as heparin drips. The intuitive interface of Sourcetable is designed specifically to handle and streamline mathematical operations, allowing healthcare professionals to perform precise calculations swiftly. Additionally, users can experiment with AI-generated data to validate their calculations, enhancing both understanding and accuracy.
Try the powerful features of Sourcetable for yourself; visit app.sourcetable.com/signup to sign up for free and transform the way you perform medical calculations.
Recommended Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.