Introduction
Understanding how to calculate base deficit is crucial for medical professionals to assess the acid-base balance in patients, particularly in situations of metabolic acidosis. This calculation helps determine the amount of excess or insufficient base in the blood, providing insights into the underlying metabolic conditions of a patient. The base deficit calculation is a core component in critical care and emergency medicine, guiding treatment strategies.
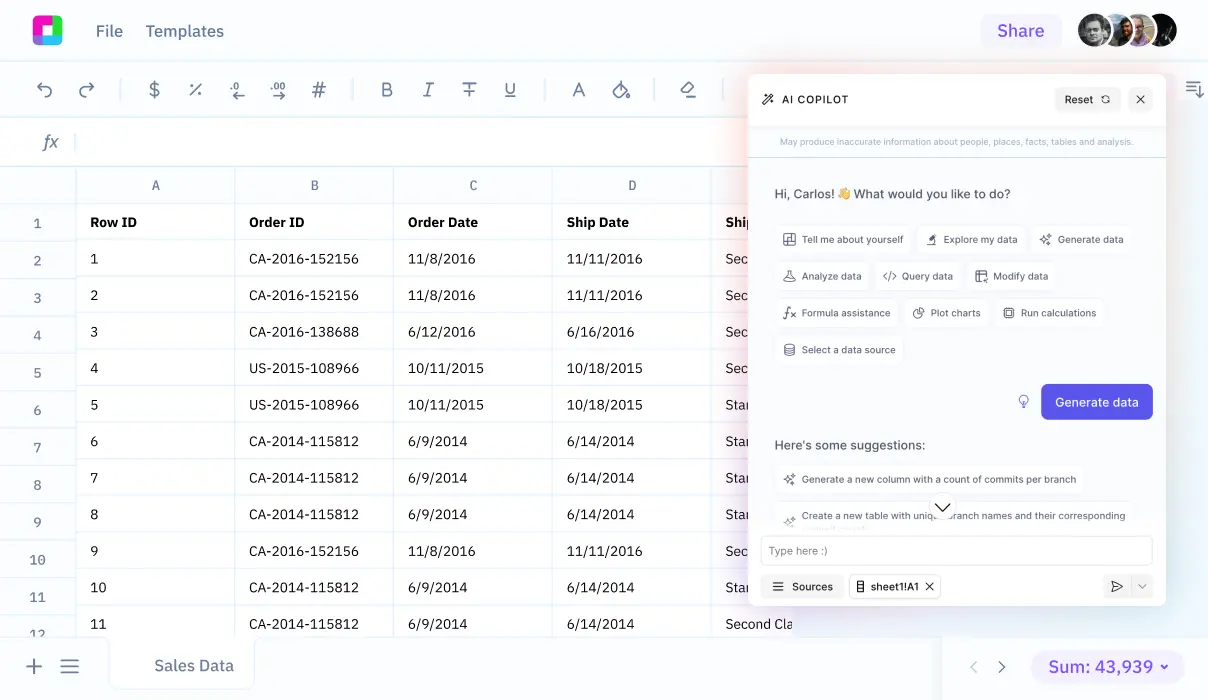
Sourcetable streamlines complex calculations like base deficit through its AI-powered spreadsheet assistant, enhancing accuracy and efficiency in medical data analysis. In the following sections, we will explore how Sourcetable lets you calculate this and more, which you can try at app.sourcetable.com/signup.
See how easy it is to base deficit with Sourcetable
How to Calculate Base Deficit
Understanding Base Deficit
Base deficit represents the amount of base required to neutralize blood acidity to a pH of 7.40 when fully oxygenated. It's key in managing acid-base disorders.
Required Data for Calculation
To determine base deficit, certain clinical measurements are necessary. Key among them are the patient's body weight, measured bicarbonate
Formulas Involved
The fundamental formula used in calculating bicarbonate deficit is
Calculating Target Change
The target change in bicarbonate levels, important for adjusting treatment, is the difference between the desired and the measured bicarbonate levels:
Putting It All Together
Once the necessary data is gathered, utilize the formulas to compute the bicarbonate deficit. This calculated deficit quantifies the required bicarbonate supplementation to correct the patient's acid-base balance effectively.
How to Calculate Base Deficit
Understanding Base Deficit
Base deficit, also known as base excess, indicates the amount of strong base required to adjust the pH of fully oxygenated blood to a normal level of 7.40. It is crucial for diagnosing conditions like diabetic ketoacidosis, lactic acidosis, and chronic kidney failure.
Formula for Base Deficit Calculation
To calculate base deficit, use the formula: Base excess = 0.02786 X pCO2 X 10^(pH - 6.1) + 13.77 X pH - 124.58. This computation helps in assessing the required amount of base to normalize the blood pH.
Calculating Bicarbonate Deficit
To determine bicarbonate deficit, start by calculating the volume of distribution factor (VD) with the formula: Vd = total body weight (kg) x [0.4 + (2.4/[HCO3-])]. Follow this by calculating the actual bicarbonate deficit: Bicarbonate deficit (mEq) = 0.5 x lean body weight (kg) x (desired [HCO3-] - measured [HCO3-]). Finally, calculate the dose of bicarbonate needed using: Bicarbonate dose (mEq) = 0.5 (L/kg) x body weight (kg) x desired increase in serum HCO3- (mEq/L).
Examples of Calculating Base Deficit
Example 1: Standard Calculation
To calculate the base deficit in a patient, subtract the patient's actual bicarbonate level from the normal bicarbonate level. If the normal level is 24 mEq/L and the patient's level is 20 mEq/L, the base deficit is 4 mEq/L.
Example 2: Using Arterial Blood Gas (ABG) Values
Consider an ABG reading with a bicarbonate (HCO3) level of 18 mEq/L. With a normal HCO3 baseline of 24 mEq/L, calculate the base deficit by subtracting the patient's HCO3 level from the normal level: 24 mEq/L - 18 mEq/L = 6 mEq/L base deficit.
Example 3: Comprehensive Blood Panel
In cases where a comprehensive metabolic panel provides bicarbonate data, use this figure to determine the base deficit. If the report shows 15 mEq/L and normal is 24 mEq/L, the deficit is 9 mEq/L.
Example 4: Impact of Fluid Administration
Post-fluid administration, if the bicarbonate levels increase from 17 mEq/L to 22 mEq/L, use the new value to reassess base deficit. With standard bicarbonate at 24 mEq/L, the deficit decreases to 2 mEq/L.
Example 5: Serial Monitoring
For ongoing treatment assessment, calculate base deficit at intervals. If initial HCO3 was 14 mEq/L and improved to 20 mEq/L on retesting, the deficit reduces from 10 mEq/L to 4 mEq/L.
Why Sourcetable is Your Ultimate Calculation Tool
Sourcetable revolutionizes calculations with its AI-powered spreadsheet technology, making it an indispensable tool for both professional and academic environments. Its ability to effortlessly handle complex calculations through simple commands helps users save time and achieve accurate results consistently.
Calculating Base Deficit with Sourcetable
Understanding base deficit is crucial in clinical settings to assess the acid-base balance in patients. Sourcetable simplifies this with its intuitive AI assistant. Just type "how to calculate base deficit" and the AI will not only compute it but also show the formulas used and the logical steps taken in the spreadsheet. This transparency in the calculation process enhances learning and understanding, especially beneficial for medical students and professionals.
Sourcetable's dual interface, combining a spreadsheet to display answers and a chat to explain methodologies, caters to diverse learning styles and operational needs. Whether it’s for study purposes or professional use, Sourcetable provides a tailored experience that bolsters efficiency and comprehension.
Choose Sourcetable for reliable, effortless, and educational calculations that support a broad spectrum of needs, from academic learning to professional decision-making.
Use Cases for Calculating Base Deficit
Predicting Mortality and Morbidity in Critical Care |
Calculation of base deficit helps predict mortality and morbidity in critically ill patients. This marker indicates the severity of acid-base disturbances, guiding clinical decisions in intensive care units. |
Assessment of Acidosis Clearance Post-Trauma |
Base deficit calculations assess the resolution of acidosis after traumatic shock. An improving base deficit suggests effective management of the patient's acid-base balance during resuscitation. |
Diagnosis of Metabolic Acidosis |
Utilizing base deficit levels, medical professionals can diagnose different types of metabolic acidosis, such as those caused by diabetic ketoacidosis or lactic acidosis. This facilitates targeted therapeutic interventions. |
Guiding Resuscitation and Therapy |
Base deficit values guide the extent and nature of resuscitation needed in emergency settings. Effective resuscitation strategies are critical for patient recovery, making base deficit a valuable measure in emergency medical services. |
Biochemical Diagnosis and Prognosis in the ICU |
In the surgical intensive care setting, both arterial and venous measurements of HCO3 can replace traditional arterial base deficit measurements to provide better diagnostic and prognostic insights. |
Management of Acid-Base Disturbances |
Base deficit calculations aid in determining the origin of acid/base disturbances, whether respiratory, metabolic, or mixed. This differentiation is crucial for appropriate management strategies. |
Frequently Asked Questions
What is the formula for calculating base deficit?
Base deficit can be calculated using different formulas, one of which is: Base excess = 0.02786 X pCO2 X 10^(pH - 6.1) + 13.77 X pH - 124.58. Another common formula is: Base excess = 0.9287 [HCO3- 24.4 + 14.83 (pH - 7.4)].
What indicates a base deficit or base excess?
A negative number in the base excess calculation indicates a base deficit, which means there is a deficiency of base in the blood. Conversely, a positive number indicates a base excess, suggesting an excess of base in the blood.
What is the normal range for base deficit or excess?
The normal value range for base deficit or excess is -2 to +2 mEq/L.
How does base deficit indicate metabolic alkalosis or acidosis?
A high positive base deficit value typically indicates metabolic alkalosis, while a low negative value indicates metabolic acidosis.
Can base deficit be calculated from a nomogram?
Yes, base deficit can be calculated from a nomogram. The Sigaard-Andersen nomogram is one commonly used tool for this purpose.
Conclusion
Calculating base deficit is crucial for understanding the acid-base balance in clinical settings. A thorough grasp of this measure helps in assessing the metabolic component of acidosis and alkalosis. It is calculated by assessing the difference between the normal and measured bicarbonate concentration, represented as (HCO_3^-).
Simplify Calculations with Sourcetable
Sourcetable, an AI-powered spreadsheet, is specifically designed to make complex calculations like base deficit straightforward. Its intuitive interface allows for quick input, computation, and analysis, perfect for healthcare professionals and researchers.
Moreover, Sourcetable offers the ability to work with AI-generated data, enabling users to simulate various scenarios and better understand the dynamics of base deficit calculations. This tool alleviates the traditional complexities associated with biochemical calculations.
Explore the full capabilities of this versatile platform by signing up for a free account at app.sourcetable.com/signup.
Recommended Guides
Connect your most-used data sources and tools to Sourcetable for seamless analysis.