Insurance claims processing can feel like navigating a maze blindfolded. One day you're cruising through straightforward auto claims, the next you're buried under complex property damage cases that seem to multiply overnight. Sound familiar?
The reality is that most insurance operations are drowning in data but starving for insights. You have spreadsheets tracking claim volumes, processing times, adjuster workloads, and fraud indicators—but connecting the dots between all these metrics feels impossible without the right analysis tools.
That's where comprehensive claims analysis becomes your secret weapon. Instead of reactive fire-fighting, you can proactively identify patterns, predict bottlenecks, and optimize your entire claims pipeline.
Why Claims Processing Analysis Matters
Transform your insurance operations from reactive to predictive with data-driven insights that improve every aspect of claims handling.
Reduce Processing Time
Identify workflow bottlenecks and streamline processes to cut average claim processing time by 30-50%.
Optimize Resource Allocation
Balance adjuster workloads and predict staffing needs based on claim volume trends and complexity patterns.
Improve Customer Satisfaction
Faster processing and proactive communication lead to higher customer satisfaction scores and retention rates.
Detect Fraud Patterns
Spot suspicious claim patterns early with automated analysis of claim amounts, frequencies, and timing anomalies.
Cost Control
Monitor claim costs by category, region, and adjuster to identify cost-saving opportunities and maintain profitability.
Regulatory Compliance
Ensure timely processing and proper documentation to meet regulatory requirements and avoid penalties.
Claims Processing Analysis in Action
See how different insurance operations use data analysis to solve common challenges and improve their claims processing efficiency.
Auto Claims Volume Surge Analysis
A regional insurer noticed their auto claims spiked 40% during winter months but couldn't predict staffing needs. By analyzing historical claim data, weather patterns, and processing times, they identified that icy road conditions in specific zip codes drove predictable claim surges. Now they pre-position adjusters and streamline simple fender-bender processing, reducing average processing time from 12 days to 6 days during peak periods.
Complex Property Damage Workflow
A commercial property insurer was losing clients due to slow processing of large claims. Analysis revealed that claims over $50K sat in review queues for an average of 8 days before assignment. By implementing priority scoring based on claim amount, policy value, and client tier, they reduced high-value claim assignment time to under 24 hours, improving client retention by 25%.
Fraud Detection Through Pattern Analysis
A health insurer suspected organized fraud but couldn't pinpoint the source. Claims analysis revealed unusual patterns: multiple claims from the same medical providers, submitted within narrow time windows, with suspiciously similar treatment codes. This analysis helped them identify a fraudulent network, saving an estimated $2.3 million in false claims and strengthening their fraud detection algorithms.
Adjuster Performance Optimization
An insurance company had wide variations in processing times between adjusters handling similar claims. Analysis showed that top performers used specific documentation techniques and followed consistent investigation sequences. By identifying these best practices and training other adjusters, they standardized processing times and improved overall claim quality scores by 35%.
Seasonal Demand Forecasting
A homeowner's insurance provider struggled with resource planning around storm seasons. Historical analysis of weather data, claim frequencies, and processing capacity revealed that hurricane season required 3x normal staffing for coastal regions, while tornado season impacted midwest operations differently. This forecasting model now guides their annual staffing and resource allocation planning.
How to Analyze Insurance Claims Processing
Follow this systematic approach to transform your claims data into actionable insights that improve efficiency and customer satisfaction.
Data Collection and Integration
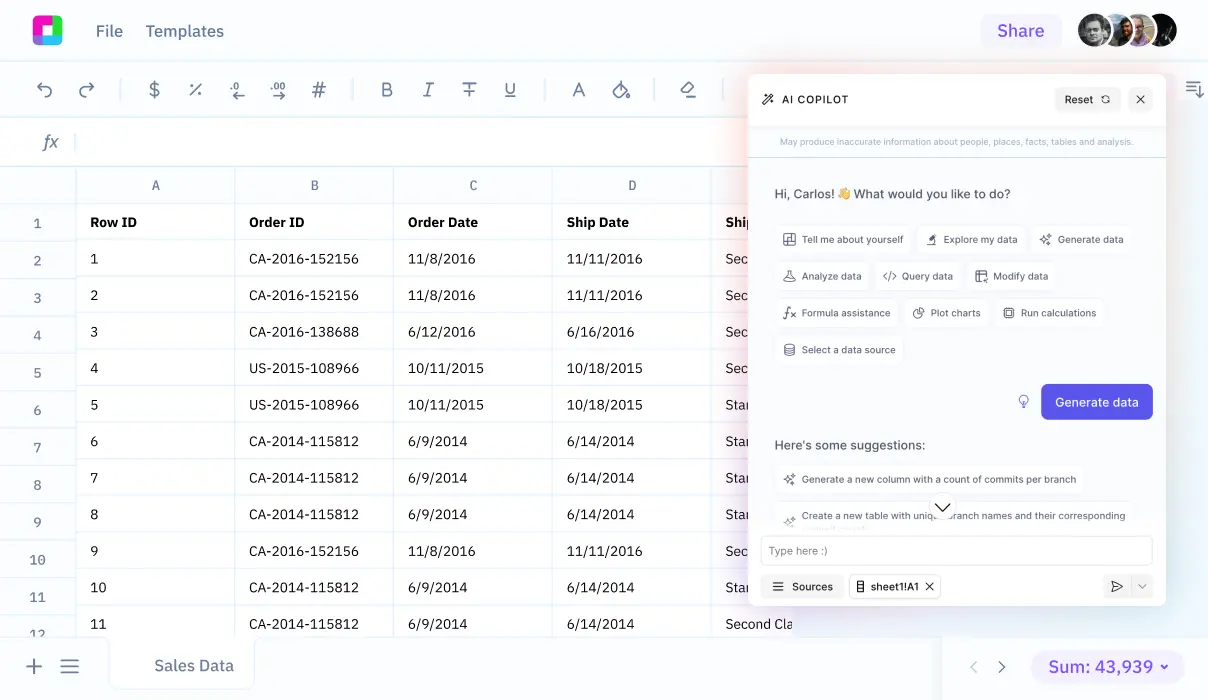
Start by gathering your claims data from multiple sources: core processing systems, adjuster reports, customer communication logs, and external data like weather or economic indicators. Import everything into Sourcetable where you can clean, standardize, and merge datasets without complex IT processes. The AI assistant helps identify data quality issues and suggests corrections automatically.
Processing Time Analysis
Create comprehensive timelines for each claim from first notice of loss through final settlement. Break down processing into stages: intake, assignment, investigation, evaluation, negotiation, and payment. Use <a href='/analysis/statistical-data-analysis'>statistical analysis</a> to identify bottlenecks, calculate average cycle times by claim type, and spot outliers that indicate process problems or exceptional cases requiring attention.
Workload and Resource Analysis
Analyze adjuster productivity, claim assignments, and capacity utilization across your team. Track metrics like claims per adjuster, average processing time by individual, case complexity scores, and quality ratings. Identify top performers and understand what makes them successful, then use those insights to optimize assignments and training programs.
Pattern Recognition and Forecasting
Use historical data to identify seasonal patterns, geographic trends, and claim type correlations. Build predictive models that forecast claim volumes based on external factors like weather, economic conditions, or calendar events. This helps with resource planning, budget forecasting, and proactive customer communication during high-volume periods.
Cost and Profitability Analysis
Examine claim costs by category, region, policy type, and processing method. Calculate the true cost of claims including processing expenses, not just payouts. Identify opportunities for cost reduction through process improvements, technology adoption, or policy adjustments. Track trends in legal costs, medical expenses, or repair costs that impact your bottom line.
Continuous Improvement Monitoring
Set up dashboards that track key performance indicators in real-time: average processing time, customer satisfaction scores, first-call resolution rates, and cost per claim. Create automated alerts for unusual patterns or performance degradation. Regular analysis helps you adapt quickly to changing conditions and maintain optimal performance.
Essential Claims Processing Metrics to Track
Successful claims analysis depends on tracking the right metrics. Here are the critical KPIs every insurance operation should monitor:
Efficiency Metrics
- Average Processing Time: Days from first notice to claim closure, broken down by claim type and complexity
- First Call Resolution Rate: Percentage of claims resolved on initial customer contact
- Reopened Claims Rate: Claims requiring additional work after initial closure
- Processing Cost per Claim: Internal costs including labor, technology, and overhead
Quality Metrics
- Customer Satisfaction Scores: Post-claim survey results and feedback trends
- Claim Accuracy Rate: Percentage of claims processed without errors or corrections
- Compliance Score: Adherence to regulatory timing and documentation requirements
- Appeal/Dispute Rate: Claims challenged by customers or requiring additional review
Resource Metrics
- Claims per Adjuster: Workload distribution and capacity utilization
- Average Case Complexity Score: Difficulty rating based on claim characteristics
- Staff Utilization Rate: Percentage of time spent on productive claim work vs. administrative tasks
- Training Hours per Quality Score: Correlation between staff development and performance
Use advanced analysis techniques to correlate these metrics and identify the factors that most impact your claims processing success.
Claims Processing Analysis FAQ
How much historical data do I need for meaningful claims analysis?
Ideally, you want at least 12-24 months of claims data to identify seasonal patterns and trends. However, you can start with as little as 3-6 months of recent data and build your analysis as you collect more information. The key is ensuring data quality and consistency rather than just volume.
What if my claims data is scattered across multiple systems?
This is common in insurance operations. Sourcetable's AI assistant can help you merge data from different sources, even when formats and field names don't match perfectly. You can import from claims management systems, spreadsheets, databases, and even PDF reports to create a comprehensive view of your operations.
How do I analyze claims processing without exposing sensitive customer information?
Focus on operational metrics rather than personal details. Analyze processing times, claim amounts, geographic regions, and claim types without using customer names or specific policy numbers. You can create anonymized datasets that protect privacy while still providing valuable insights for process improvement.
Can I predict which claims will take longer to process?
Yes, by analyzing historical patterns. Factors like claim amount, type of loss, policy coverage, customer history, and even external factors like weather or economic conditions can help predict processing complexity. Build scoring models that flag potentially complex claims early so you can allocate appropriate resources.
How do I measure the ROI of claims processing improvements?
Track before-and-after metrics including processing costs per claim, customer satisfaction scores, staff productivity, and regulatory compliance rates. Calculate the cost savings from reduced processing time, fewer errors, and improved customer retention. Most operations see 15-30% improvement in efficiency within the first year of systematic analysis.
What's the best way to identify fraud patterns in claims data?
Look for statistical anomalies: unusual claim frequencies from specific providers, geographic clusters of similar claims, timing patterns that suggest coordination, or claim amounts that cluster around policy limits. Statistical analysis can automatically flag outliers for investigation while protecting legitimate claims from unnecessary delays.
How often should I update my claims processing analysis?
Monitor key metrics daily or weekly for operational management, but conduct comprehensive analysis monthly or quarterly. Seasonal businesses might need more frequent analysis during peak periods. Set up automated alerts for significant changes in processing times, costs, or quality metrics so you can respond quickly to emerging issues.
Can I benchmark my claims processing against industry standards?
While specific benchmarks vary by insurance type and company size, common targets include: auto claims processed in 7-10 days, property claims in 15-30 days, and customer satisfaction scores above 85%. Focus more on your own improvement trends rather than absolute benchmarks, as your specific market and policy mix create unique challenges.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us