Why Healthcare Risk Management Analysis Matters
Every day, healthcare organizations face a complex web of risks—from patient safety incidents to regulatory compliance gaps. Traditional risk management often relies on reactive reporting and manual analysis, leaving critical patterns hidden in the data.
With statistical analysis and AI-powered insights, you can transform how your organization identifies, assesses, and mitigates healthcare risks. Turn your data into a proactive shield that protects patients, staff, and your organization's mission.
Transform Risk Management with Data-Driven Insights
See how AI-powered analysis revolutionizes healthcare risk management
Early Risk Detection
Identify potential safety issues before they become incidents. Analyze patterns across departments, shifts, and patient populations to spot risks in real-time.
Predictive Analytics
Forecast risk trends and allocate resources proactively. Use historical data to predict where and when risks are most likely to occur.
Compliance Monitoring
Track regulatory compliance metrics automatically. Generate reports that demonstrate adherence to Joint Commission, CMS, and other regulatory standards.
Cost Impact Analysis
Quantify the financial impact of risks and mitigation strategies. Make data-driven decisions about resource allocation and prevention investments.
Real-time Dashboards
Monitor key risk indicators with live dashboards. Get instant alerts when metrics cross critical thresholds or unusual patterns emerge.
Cross-department Integration
Combine data from multiple systems and departments. Create a comprehensive view of organizational risk that breaks down silos.
Healthcare Risk Analysis in Action
See how different healthcare organizations use data analysis to improve safety and outcomes
Patient Fall Prevention Analysis
A regional medical center analyzed two years of incident reports, staffing data, and patient acuity scores. They discovered that falls increased 40% during evening shifts when nurse-to-patient ratios exceeded 1:6. By adjusting staffing patterns and implementing targeted interventions, they reduced falls by 35% within six months.
Medication Error Pattern Detection
A hospital system combined pharmacy data, electronic health records, and incident reports to identify medication error hotspots. They found that 60% of errors occurred with sound-alike drugs during shift changes. This led to new protocols that reduced medication errors by 50% in high-risk units.
Surgical Site Infection Prediction
An orthopedic surgery center analyzed patient demographics, procedure types, and environmental factors to predict infection risk. Their model identified patients with 3x higher infection risk, enabling targeted prophylaxis protocols that reduced infections by 45%.
Emergency Department Capacity Planning
A trauma center analyzed five years of admission data, weather patterns, and local events to predict surge capacity needs. Their predictive model helped them prepare for peak demand periods, reducing average wait times by 25% and improving patient satisfaction scores.
Staff Burnout Risk Assessment
A nursing department tracked overtime hours, patient acuity, and staff satisfaction surveys to identify burnout risk factors. They discovered that nurses working more than 50 hours per week had 3x higher turnover rates, leading to policy changes that improved retention by 30%.
Financial Risk from Readmissions
A health system analyzed readmission patterns across different conditions and identified that diabetic patients with certain social determinants had 2x higher readmission rates. Targeted interventions reduced preventable readmissions by 28% and improved quality scores.
Your Path to Data-Driven Risk Management
Transform your healthcare risk management in four simple steps
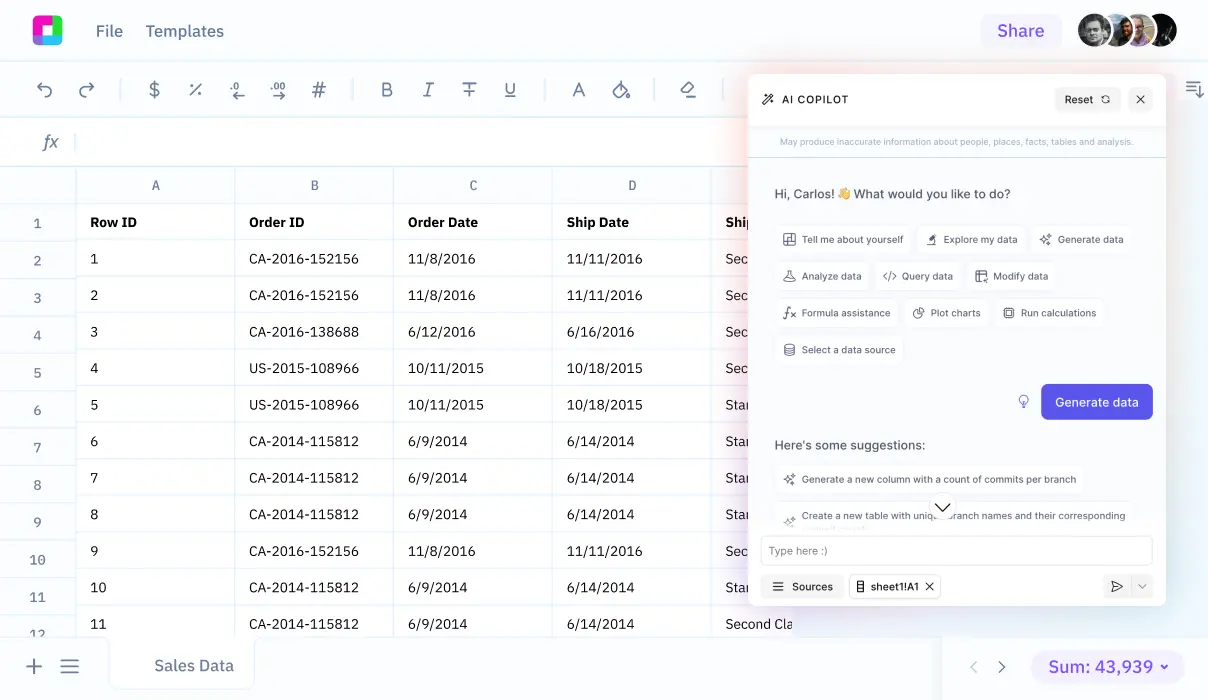
Connect Your Data Sources
Import data from your EHR, incident reporting systems, staffing databases, and quality metrics. Sourcetable handles multiple formats and automatically structures your data for analysis.
Identify Risk Patterns
Use AI-powered analysis to uncover hidden patterns in your data. Discover correlations between staffing levels, patient acuity, environmental factors, and risk events that manual analysis might miss.
Build Predictive Models
Create models that predict risk likelihood based on current conditions. Set up automated alerts for high-risk scenarios and track key performance indicators in real-time.
Implement and Monitor
Deploy risk mitigation strategies based on your insights. Continuously monitor outcomes and refine your approach with updated data and feedback loops.
Essential Healthcare Risk Analyses
Patient Safety Analytics
Track and analyze adverse events, near misses, and safety indicators. Use trend analysis to identify emerging safety concerns before they impact patient care. Monitor hand hygiene compliance, medication administration accuracy, and other critical safety metrics.
Operational Risk Assessment
Analyze staffing patterns, equipment failures, and workflow bottlenecks that create operational risks. Identify correlations between operational metrics and patient outcomes to optimize both efficiency and safety.
Financial Risk Modeling
Assess financial exposure from malpractice claims, regulatory penalties, and quality-based payment adjustments. Use scenario analysis to model the impact of different risk mitigation strategies.
Compliance Monitoring
Track adherence to clinical protocols, regulatory requirements, and accreditation standards. Set up automated monitoring for key compliance indicators and generate audit-ready reports.
Population Health Risk Stratification
Segment patient populations by risk factors to enable targeted interventions. Analyze social determinants, clinical indicators, and utilization patterns to identify high-risk cohorts.
Connect All Your Healthcare Data
Effective risk management requires a comprehensive view of your organization. Sourcetable integrates data from multiple sources to give you the complete picture:
Our AI automatically detects relationships between disparate data sources, helping you uncover risk factors that span multiple systems and departments.
Healthcare Risk Management Analysis FAQ
How does AI improve healthcare risk management compared to traditional methods?
AI can process vast amounts of data from multiple sources simultaneously, identifying patterns and correlations that humans might miss. It provides predictive capabilities, real-time monitoring, and can analyze complex interactions between factors like staffing, patient acuity, and environmental conditions. This enables proactive risk management rather than reactive responses.
What types of healthcare data can be analyzed for risk management?
You can analyze virtually any healthcare data including EHR records, incident reports, staffing data, financial metrics, patient satisfaction scores, regulatory compliance data, equipment maintenance logs, and environmental monitoring data. The key is combining multiple data sources for comprehensive risk assessment.
How quickly can we see results from implementing data-driven risk management?
Many organizations see initial insights within days of data integration. Significant risk reduction typically occurs within 3-6 months as predictive models are refined and interventions are implemented. The timeline depends on data quality, organizational readiness, and the complexity of risk factors being addressed.
Is this approach suitable for small healthcare practices or only large health systems?
Data-driven risk management scales to organizations of all sizes. Small practices can focus on key risk areas like patient safety incidents and compliance monitoring, while larger systems can implement comprehensive enterprise-wide risk management. The tools and complexity can be tailored to your organization's size and needs.
How do we ensure patient privacy and HIPAA compliance when analyzing healthcare data?
All analysis can be performed with de-identified or aggregated data to maintain HIPAA compliance. Sourcetable includes built-in privacy protections and can work with your IT security team to ensure all data handling meets regulatory requirements. Many analyses focus on patterns and trends rather than individual patient information.
What's the ROI of implementing healthcare risk management analysis?
ROI comes from multiple sources: reduced malpractice claims, improved quality scores, better regulatory compliance, decreased staff turnover, and optimized resource allocation. Many organizations see cost savings of 10-30% in risk-related expenses within the first year, plus improvements in patient outcomes and satisfaction.
Can this analysis help with Joint Commission preparation and other accreditation processes?
Yes, absolutely. Data-driven risk management creates comprehensive documentation of safety initiatives, tracks performance improvement over time, and generates the reports needed for accreditation surveys. It helps demonstrate a culture of safety and continuous improvement that accrediting bodies value.
How do we get staff buy-in for data-driven risk management initiatives?
Start by demonstrating quick wins with analyses that solve immediate pain points. Show how data supports clinical decision-making rather than replacing clinical judgment. Involve frontline staff in identifying risk factors and interpreting results. Training and clear communication about benefits help build support across the organization.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us