Healthcare revenue cycle management is like conducting an orchestra - every instrument must play in perfect harmony to create beautiful music. When your patient registration, coding, billing, and collections processes work seamlessly together, your organization's financial health flourishes. But when one section falls out of tune, the entire performance suffers.
Traditional revenue cycle analysis often feels like trying to solve a puzzle with missing pieces. You have data scattered across multiple systems, metrics that don't tell the full story, and bottlenecks that seem to appear out of nowhere. With AI-powered analysis, you can finally see the complete picture and make data-driven decisions that transform your revenue cycle performance.
Why Healthcare Revenue Cycle Analysis Matters
Transform your financial operations with comprehensive revenue cycle insights
Reduce Days in A/R
Identify payment delays and streamline collection processes to accelerate cash flow. Track aging reports and pinpoint accounts that need immediate attention.
Improve Clean Claim Rates
Analyze denial patterns and coding accuracy to increase first-pass claim acceptance rates. Reduce costly rework and administrative overhead.
Optimize Patient Experience
Track patient satisfaction scores alongside financial metrics to ensure quality care doesn't suffer while improving revenue performance.
Enhance Staff Productivity
Monitor workload distribution and identify training opportunities to maximize your team's efficiency across all revenue cycle functions.
Predict Cash Flow
Use historical patterns and current pipeline data to forecast revenue and plan for seasonal variations or unexpected changes.
Benchmark Performance
Compare your metrics against industry standards and identify opportunities for improvement across all revenue cycle stages.
Your Revenue Cycle Analysis Journey
From data chaos to financial clarity in four simple steps
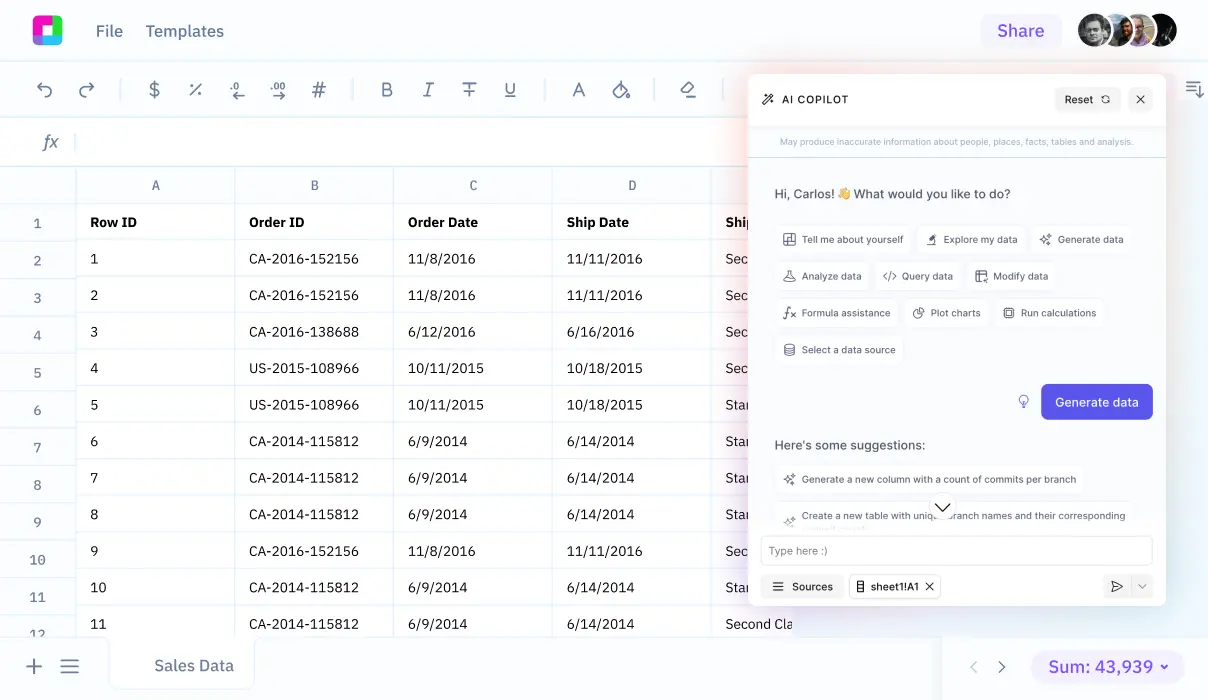
Connect Your Systems
Import data from your EHR, practice management system, and billing software. Sourcetable automatically consolidates information from multiple sources into one unified view.
Analyze Key Metrics
Track critical KPIs like days in A/R, clean claim rates, denial percentages, and collection ratios. AI identifies trends and anomalies that require attention.
Identify Bottlenecks
Pinpoint exactly where your revenue cycle slows down. Whether it's registration errors, coding delays, or collection issues, you'll know where to focus your efforts.
Take Action
Get specific recommendations for improvement. From staff training needs to process optimizations, turn insights into measurable financial results.
Revenue Cycle Analysis in Action
See how healthcare organizations use data analysis to solve common challenges
Emergency Department Throughput Analysis
A regional medical center analyzed patient flow data to identify ED bottlenecks. By tracking registration times, triage efficiency, and discharge processes, they reduced average length of stay by 23% and improved patient satisfaction scores while maintaining billing accuracy. The analysis revealed that insurance verification delays were the primary cause of extended stays.
Surgical Services Revenue Optimization
A multi-specialty surgical practice used revenue cycle analysis to improve OR utilization and billing efficiency. By analyzing case scheduling patterns, surgeon productivity, and post-operative billing cycles, they increased monthly revenue by 18% while reducing administrative costs. The key insight was optimizing block scheduling based on historical case duration data.
Specialty Clinic Denial Management
A dermatology clinic group struggling with high denial rates implemented comprehensive claims analysis. By tracking denial reasons, payer-specific patterns, and coding accuracy across providers, they reduced denial rates from 12% to 4% within six months. The analysis identified specific CPT codes that required additional documentation.
Rural Hospital Cash Flow Forecasting
A critical access hospital used revenue cycle analytics to predict seasonal cash flow variations. By analyzing historical payment patterns, seasonal patient volumes, and payer mix changes, they improved cash flow forecasting accuracy by 35% and avoided potential cash shortages during slow periods.
Mental Health Practice Efficiency Study
A behavioral health organization analyzed appointment scheduling, no-show rates, and billing cycles to optimize resource allocation. The analysis revealed that certain appointment times had 40% higher no-show rates, allowing them to implement targeted reminder strategies and improve overall utilization by 28%.
Oncology Center Treatment Pathway Analysis
A cancer treatment center tracked patient journeys from initial consultation through treatment completion to identify revenue optimization opportunities. By analyzing treatment protocols, billing patterns, and patient outcomes, they improved revenue per patient by 15% while maintaining quality metrics.
Key Revenue Cycle Metrics to Track
Successful revenue cycle management requires monitoring the right metrics at the right frequency. Here are the essential KPIs every healthcare organization should track:
Financial Performance Indicators
- Days in Accounts Receivable (A/R): Average time from service delivery to payment collection
- Net Collection Rate: Percentage of expected payments actually collected
- Cost to Collect: Administrative costs as a percentage of total collections
- Bad Debt Rate: Percentage of gross charges written off as uncollectible
Operational Efficiency Metrics
- Clean Claim Rate: Percentage of claims processed without errors on first submission
- Denial Rate: Percentage of claims initially denied by payers
- Time to Bill: Average days from service delivery to claim submission
- Registration Accuracy: Percentage of patient registrations completed without errors
Patient Experience Indicators
- Patient Satisfaction Scores: Ratings for billing and financial counseling services
- Point-of-Service Collections: Percentage of patient responsibility collected at time of service
- Payment Plan Adoption: Rate at which patients enroll in structured payment programs
- Financial Counseling Effectiveness: Percentage of patients who understand their financial responsibility
The magic happens when you analyze these metrics together rather than in isolation. For example, a slight decrease in clean claim rate might seem minor, but when combined with increased denial rates and longer days in A/R, it signals a significant trend that needs immediate attention.
Advanced Revenue Cycle Analysis Techniques
Once you've mastered basic revenue cycle metrics, advanced analytical techniques can unlock even deeper insights into your financial performance:
Cohort Analysis for Patient Populations
Group patients by similar characteristics (insurance type, service line, geographic location) and track their revenue cycle performance over time. This reveals patterns like which payers consistently delay payments or which service lines generate the highest margins.
Predictive Modeling for Denials
Use historical denial data to predict which claims are most likely to be denied before submission. This allows for proactive claim scrubbing and reduces the costly denial-appeal cycle.
Provider Performance Benchmarking
Compare individual provider performance across revenue cycle metrics while accounting for case mix differences. Identify top performers and understand what makes them successful so you can replicate their practices.
Seasonal Trend Analysis
Healthcare revenue often follows predictable seasonal patterns due to insurance deductible cycles, elective procedure scheduling, and holiday impacts. Understanding these patterns helps with cash flow planning and staffing decisions.
These advanced techniques require sophisticated data analysis capabilities, but they can uncover insights that translate directly into improved financial performance. With AI-powered spreadsheet tools, even complex analyses become accessible to healthcare finance teams.
Frequently Asked Questions
How often should we perform revenue cycle analysis?
Key metrics should be monitored daily or weekly, with comprehensive analysis performed monthly. Critical indicators like days in A/R and denial rates need frequent attention, while trend analysis and benchmarking can be done quarterly. The frequency depends on your organization's size and complexity.
What's the biggest mistake healthcare organizations make in revenue cycle analysis?
The most common mistake is analyzing metrics in isolation rather than understanding how they interconnect. For example, focusing solely on reducing days in A/R without considering clean claim rates or patient satisfaction can lead to aggressive collection practices that damage patient relationships and long-term revenue.
How do we benchmark our performance against industry standards?
Industry benchmarks vary by organization type, size, and specialty. Critical access hospitals have different targets than large health systems. Use data from organizations similar to yours and consider factors like payer mix, patient demographics, and service offerings when comparing performance.
Can revenue cycle analysis help with value-based care contracts?
Absolutely. Revenue cycle analysis is crucial for value-based care success. You need to track quality metrics alongside financial performance, monitor patient outcomes, and understand the total cost of care. This analysis helps identify opportunities to improve both financial and clinical outcomes.
What data do we need to get started with revenue cycle analysis?
Start with basic financial data: charges, payments, adjustments, and write-offs by date, provider, and service line. Add patient demographic information, insurance details, and claim status data. As you progress, incorporate operational data like appointment scheduling, no-show rates, and staff productivity metrics.
How can we ensure data accuracy in our revenue cycle analysis?
Implement data validation rules at the point of entry, perform regular audits of key data fields, and establish clear definitions for all metrics. Create automated checks for common data quality issues like missing information or inconsistent coding. Regular staff training on data entry standards is also essential.
What's the ROI of implementing comprehensive revenue cycle analysis?
Organizations typically see 3-8% improvement in net revenue within the first year of implementing systematic revenue cycle analysis. This comes from reduced denials, faster collections, improved coding accuracy, and better resource allocation. The exact ROI depends on your current performance and implementation approach.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us