Healthcare quality metrics are the compass that guides patient care excellence. Yet for many healthcare professionals, turning raw data into meaningful insights feels like navigating a maze blindfolded. Patient satisfaction scores, readmission rates, clinical indicators – they're all there in your spreadsheets, but extracting the story they tell requires more than basic calculations.
Whether you're a quality improvement coordinator tracking HCAHPS scores, a clinical manager analyzing infection rates, or a healthcare analyst preparing board reports, you need tools that understand the complexity of healthcare data. That's where intelligent analysis transforms overwhelming datasets into clear, actionable insights that drive better patient outcomes.
Why Healthcare Quality Analysis Matters
Transform your quality improvement initiatives with data-driven insights that make a real difference in patient care
Comprehensive Quality Tracking
Monitor patient satisfaction, clinical outcomes, safety indicators, and operational metrics in one unified dashboard that tells the complete quality story
Regulatory Compliance Made Simple
Stay ahead of CMS requirements, Joint Commission standards, and quality reporting mandates with automated calculations and standardized metrics
Predictive Quality Insights
Identify at-risk patients, predict readmission likelihood, and spot quality trends before they become problems using advanced analytics
Benchmarking & Comparisons
Compare your performance against national averages, peer institutions, and historical trends to understand where you excel and where to focus improvement efforts
Action-Oriented Reporting
Generate executive summaries, department scorecards, and improvement action plans that turn data into concrete steps for better patient care
Real-Time Quality Monitoring
Track quality indicators as they happen, set up alerts for critical thresholds, and respond to quality issues before they impact patient outcomes
Healthcare Quality Analysis in Action
See how healthcare organizations use quality metrics analysis to drive meaningful improvements in patient care and operational performance
Patient Satisfaction Score Analysis
A regional hospital system tracks HCAHPS scores across 12 facilities, identifying communication gaps that led to targeted staff training and a 15% improvement in patient satisfaction within six months. The analysis revealed specific units and shifts with lower scores, enabling focused interventions.
Readmission Rate Reduction Initiative
A medical center analyzes 30-day readmission patterns across different diagnoses, discovering that patients discharged on Fridays had 23% higher readmission rates. This insight led to enhanced weekend discharge planning protocols and reduced overall readmissions by 18%.
Infection Control Performance Tracking
An infection prevention team monitors hospital-acquired infection rates across ICUs, surgical units, and medical floors. By correlating infection data with staffing levels, hand hygiene compliance, and patient acuity, they identified optimal staffing ratios that maintain quality while controlling costs.
Emergency Department Quality Metrics
An ED quality manager tracks door-to-provider times, patient throughput, and satisfaction scores to identify bottlenecks. The analysis revealed that triage process improvements could reduce wait times by 35% during peak hours while maintaining care quality standards.
Surgical Quality Outcome Analysis
A surgical department analyzes complications, length of stay, and patient-reported outcomes across different procedures and surgeons. This comprehensive view helps identify best practices, optimize surgical protocols, and improve patient outcomes through data-driven quality improvement.
Medication Safety Performance Review
A pharmacy quality team tracks medication errors, near-misses, and adverse drug events across hospital units. By analyzing patterns and root causes, they implement targeted interventions that reduce medication-related incidents by 40% while improving patient safety culture.
How Healthcare Quality Analysis Works
Follow this systematic approach to transform your quality data into actionable insights that drive better patient outcomes
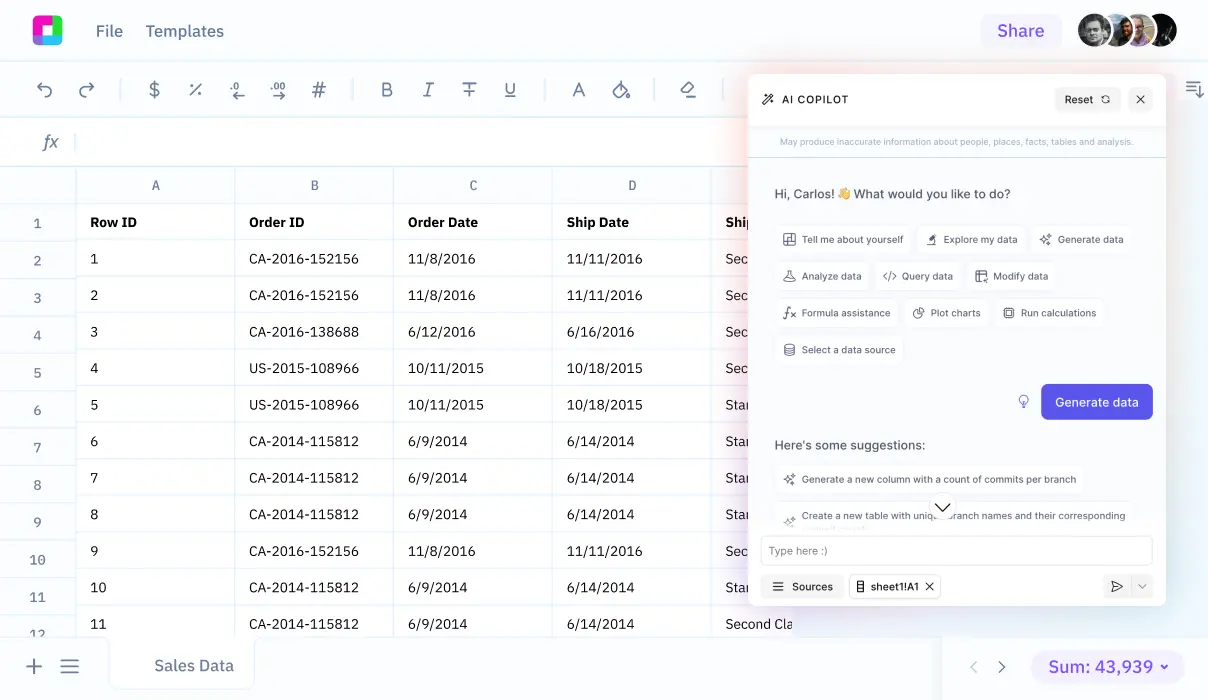
Data Collection & Integration
Import quality data from EMRs, patient satisfaction surveys, incident reports, and regulatory databases. Combine clinical, operational, and patient experience metrics into a comprehensive quality dataset that provides the complete picture.
Quality Indicator Calculation
Calculate standardized quality metrics including patient safety indicators, clinical outcome measures, patient experience scores, and operational efficiency ratios. Use industry-standard formulas and benchmarks for accurate comparisons.
Trend Analysis & Benchmarking
Analyze quality trends over time, compare performance against national benchmarks and peer institutions, and identify areas of excellence or concern. Spot patterns that might indicate systemic issues or improvement opportunities.
Root Cause Investigation
Drill down into quality issues to understand underlying causes. Correlate quality metrics with staffing patterns, patient acuity, seasonal variations, and process changes to identify improvement opportunities.
Action Plan Development
Create targeted improvement initiatives based on data insights. Prioritize interventions by impact potential, resource requirements, and patient safety considerations to maximize quality improvement effectiveness.
Monitoring & Reporting
Track improvement progress with ongoing monitoring, generate regular quality reports for leadership and regulatory bodies, and maintain accountability through transparent quality performance dashboards.
Essential Healthcare Quality Metrics to Track
Successful healthcare quality analysis focuses on the metrics that matter most for patient outcomes and organizational performance. Here are the core categories every quality program should monitor:
Patient Safety Indicators
Clinical Outcome Measures
Patient Experience Scores
Healthcare Quality Analysis FAQ
How do I ensure my quality metrics comply with regulatory requirements?
Focus on standardized quality indicators used by CMS, Joint Commission, and other regulatory bodies. Use established calculation methods, maintain proper documentation, and regularly validate your data against published benchmarks. Consider working with quality consultants to ensure compliance with evolving requirements.
What's the best way to present quality data to different audiences?
Tailor your presentation to the audience's needs. Executive dashboards should focus on high-level trends and key performance indicators. Department managers need operational details and actionable insights. Clinical staff benefit from peer comparisons and practice-specific metrics. Use visual tools like scorecards, trend charts, and benchmark comparisons.
How often should I analyze healthcare quality metrics?
Monitor critical safety indicators daily or weekly, review operational quality metrics monthly, and conduct comprehensive quality assessments quarterly. Patient satisfaction and clinical outcomes can be tracked monthly, while annual reviews should focus on long-term trends and strategic quality improvements.
How do I identify which quality metrics are most important for my organization?
Start with regulatory requirements and patient safety priorities, then add metrics aligned with your strategic goals. Consider your patient population, service lines, and quality improvement initiatives. Focus on metrics where you can take action based on the results, and gradually expand your measurement program as capabilities grow.
What should I do when quality metrics show concerning trends?
Investigate immediately to understand root causes, engage relevant clinical and operational teams, and develop targeted action plans. Use data to identify patterns, compare with peer institutions, and implement evidence-based interventions. Establish monitoring protocols to track improvement and prevent recurrence.
How can I use quality data to drive meaningful improvements?
Connect quality metrics to specific processes and outcomes, identify improvement opportunities through data analysis, and engage frontline staff in developing solutions. Use quality data to support business cases for resources, track intervention effectiveness, and celebrate successes to maintain momentum for continuous improvement.
Advanced Healthcare Quality Analytics
Moving beyond basic quality reporting, advanced analytics can unlock deeper insights and predictive capabilities that transform quality improvement from reactive to proactive. Here's how sophisticated analysis techniques enhance healthcare quality programs:
Predictive Quality Modeling
Use historical quality data to predict future risks and outcomes. Identify patients at high risk for readmission, predict which units might experience quality issues, and forecast resource needs for quality improvement initiatives. Machine learning algorithms can detect subtle patterns that traditional analysis might miss.
Statistical Process Control
Apply control charts and statistical methods to distinguish between normal variation and significant changes in quality performance. This approach helps quality teams focus on true quality issues rather than random fluctuations, improving the efficiency of improvement efforts.
Multi-dimensional Quality Analysis
Analyze quality from multiple perspectives simultaneously – clinical outcomes, patient experience, staff satisfaction, and operational efficiency. This holistic view reveals connections between different quality dimensions and helps optimize overall healthcare delivery.
Real-time Quality Intelligence
Implement dashboards and alert systems that provide immediate feedback on quality performance. Real-time monitoring enables rapid response to quality issues and supports continuous quality improvement culture throughout the organization.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us