The Healthcare Operations Challenge
Picture this: It's 2 AM, and you're staring at a spreadsheet filled with patient wait times, staff schedules, and resource utilization data. The board meeting is tomorrow, and you need to present actionable insights on operational efficiency. Sound familiar?
Healthcare operations professionals face unique challenges. You're juggling patient satisfaction scores, staff productivity metrics, equipment utilization rates, and cost optimization—all while ensuring quality care remains the top priority. Traditional analysis tools often fall short when dealing with the complexity and urgency of healthcare data.
That's where intelligent analysis comes in. With AI-powered data analysis, you can transform raw operational data into strategic insights that drive real improvements in patient care and organizational efficiency.
Why Healthcare Operations Teams Choose Data-Driven Analysis
Transform your healthcare operations with insights that matter to patients and bottom lines alike.
Reduce Patient Wait Times
Identify bottlenecks in patient flow and optimize scheduling to improve satisfaction scores by up to 40%.
Optimize Staff Allocation
Balance workloads across departments and shifts, reducing overtime costs while maintaining quality care standards.
Improve Resource Utilization
Track equipment usage, room occupancy, and supply consumption to maximize ROI on healthcare investments.
Enhance Quality Metrics
Monitor patient outcomes, readmission rates, and satisfaction scores to identify improvement opportunities.
Streamline Financial Operations
Analyze revenue cycles, insurance claims, and operational costs to improve financial performance.
Predict Demand Patterns
Use historical data to forecast patient volumes and adjust staffing and resources proactively.
Healthcare Operations Analysis in Action
See how healthcare professionals are using data analysis to solve real operational challenges.
Emergency Department Flow Optimization
A major hospital reduced average patient wait times from 3.2 hours to 1.8 hours by analyzing triage patterns, staffing levels, and treatment protocols. The analysis revealed that 60% of delays occurred during shift changes, leading to a staggered shift schedule that improved patient flow.
Operating Room Efficiency Analysis
A surgical center increased OR utilization from 68% to 89% by analyzing surgery duration patterns, equipment setup times, and scheduling gaps. The data showed that certain procedure combinations could be optimized, resulting in 4 additional surgeries per week.
Nursing Staff Productivity Assessment
A regional healthcare network reduced nursing overtime costs by 28% while improving patient satisfaction scores. Analysis of patient acuity levels, admission patterns, and staff competencies enabled better shift planning and skill-based assignments.
Supply Chain Cost Optimization
A hospital system saved $2.3M annually by analyzing supply usage patterns, vendor performance, and inventory turnover rates. The analysis identified opportunities to standardize products and negotiate better contracts with high-volume suppliers.
Patient Readmission Prevention
A healthcare provider reduced 30-day readmission rates by 23% by analyzing patient demographics, discharge protocols, and follow-up care patterns. The insights led to targeted interventions for high-risk patient populations.
Your Healthcare Operations Analysis Workflow
From data collection to actionable insights in four simple steps.
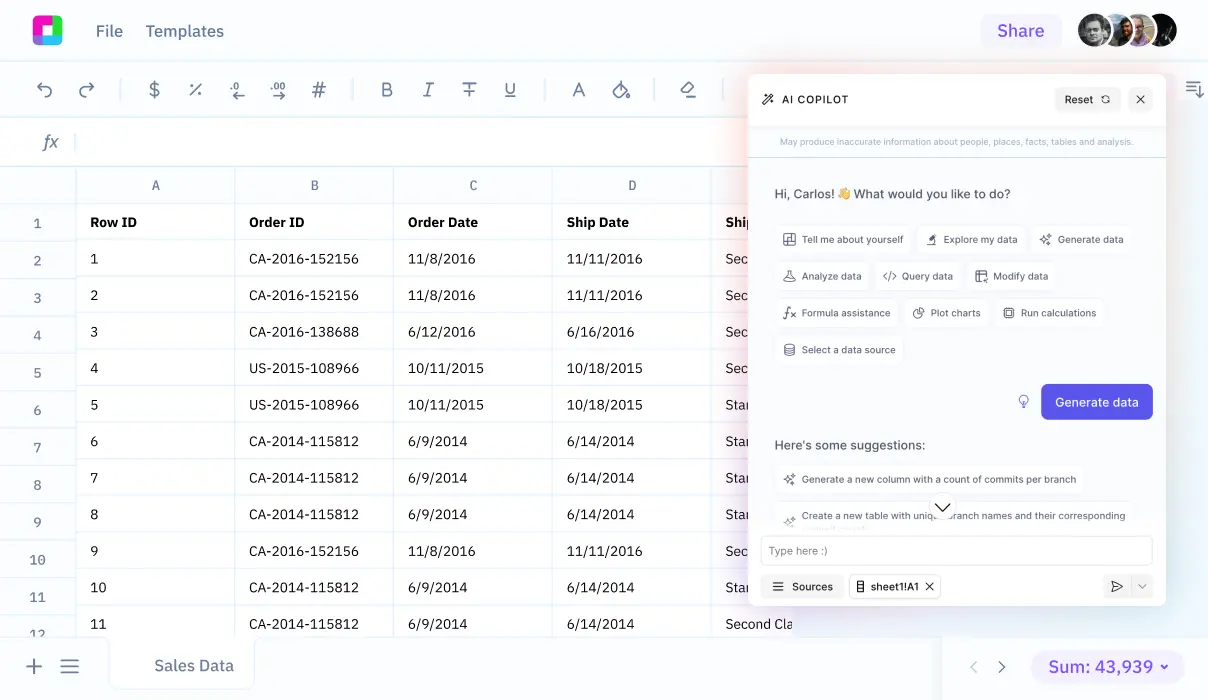
Data Integration
Connect your EHR systems, scheduling software, and operational databases. Import patient flow data, staffing records, and financial metrics into a unified analysis environment.
Pattern Recognition
Use AI-powered analysis to identify trends in patient volumes, staff productivity, and resource utilization. Discover correlations between operational factors and patient outcomes.
Performance Benchmarking
Compare your metrics against industry standards and best practices. Identify areas where your operations exceed benchmarks and opportunities for improvement.
Action Planning
Generate specific recommendations for operational improvements. Create implementation roadmaps with measurable goals and timeline tracking for each initiative.
Essential Healthcare Operations Metrics to Track
Successful healthcare operations analysis focuses on metrics that directly impact patient care and organizational sustainability. Here are the key performance indicators that matter most:
Patient Flow Metrics
Staff Productivity Indicators
Financial Performance Metrics
When you analyze these metrics together, patterns emerge that reveal the true drivers of operational efficiency. For example, a spike in patient wait times might correlate with increased LWBS rates and decreased satisfaction scores, pointing to specific process improvements needed.
Integrating with Your Healthcare Technology Stack
Healthcare operations analysis is most effective when it connects seamlessly with your existing technology infrastructure. Modern analysis tools should integrate with your current systems without disrupting workflows.
Electronic Health Records (EHR) Integration
Your EHR system contains a wealth of operational data—patient demographics, treatment times, provider notes, and outcome metrics. By connecting this data to your analysis platform, you can track patient journey efficiency and identify bottlenecks in care delivery processes.
Scheduling and Resource Management Systems
Staff scheduling, room assignments, and equipment booking systems generate valuable data about resource utilization. Analysis of this information reveals patterns in demand, helps optimize staff allocation, and identifies opportunities to improve facility usage.
Financial and Billing Systems
Revenue cycle data, insurance claims, and cost accounting systems provide the financial context for operational decisions. Understanding the cost implications of operational changes ensures that efficiency improvements also support financial sustainability.
The key is choosing analysis tools that can handle the complexity and sensitivity of healthcare data while providing the flexibility to work with various data sources and formats. Look for solutions that support Excel compatibility and can process both structured and unstructured data types.
Frequently Asked Questions
How do I ensure patient data privacy during operations analysis?
Healthcare operations analysis should always use de-identified or aggregated data that complies with HIPAA regulations. Focus on operational metrics like wait times, resource utilization, and workflow efficiency rather than individual patient information. Use secure, healthcare-compliant analysis platforms that include proper access controls and audit trails.
What's the typical ROI timeline for healthcare operations analysis initiatives?
Most healthcare organizations see initial improvements within 3-6 months of implementing data-driven operations analysis. Quick wins like optimized scheduling or improved patient flow can reduce wait times and increase satisfaction scores immediately. Larger initiatives like staff optimization or supply chain improvements typically show significant ROI within 12-18 months.
How can small healthcare practices benefit from operations analysis?
Small practices can achieve significant improvements by focusing on key metrics like appointment scheduling efficiency, patient no-show rates, and staff productivity. Even basic analysis of patient flow patterns and resource utilization can identify opportunities to reduce costs and improve patient satisfaction without requiring large technology investments.
What data sources are most important for healthcare operations analysis?
The most valuable data sources include patient scheduling systems, EHR workflow data, staff scheduling records, financial systems, and patient satisfaction surveys. Quality metrics like readmission rates, infection rates, and safety indicators are also crucial for comprehensive operations analysis.
How do I get staff buy-in for operations analysis initiatives?
Start with small, focused projects that address specific pain points staff experience daily. Show how analysis can reduce their workload or improve patient care rather than just cutting costs. Involve frontline staff in identifying problems and reviewing findings to ensure recommendations are practical and implementable.
Can operations analysis help with regulatory compliance?
Yes, operations analysis can help track compliance-related metrics like infection rates, medication errors, patient safety indicators, and quality measures required by regulatory bodies. Automated reporting and trend analysis can help identify compliance risks before they become issues and demonstrate continuous improvement efforts.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us