Healthcare facility design isn't just about aesthetics—it's about saving lives. Every corridor width, every room placement, every workflow intersection can mean the difference between efficient care delivery and dangerous delays. That's where intelligent layout analysis transforms good intentions into measurable outcomes.
Picture this: A busy emergency department where nurses walk an extra 2.3 miles per shift because supply rooms are poorly positioned. Or an ICU where critical equipment delays occur because the layout creates bottlenecks during shift changes. These aren't abstract problems—they're daily realities that operational efficiency analysis can solve.
Why Healthcare Layout Analysis Matters
Discover the key benefits
Patient Safety Enhancement
Identify blind spots, reduce fall risks, and optimize sight lines for better patient monitoring. Data-driven layouts can reduce safety incidents by up to 35%.
Staff Efficiency Optimization
Minimize unnecessary movement, reduce fatigue, and streamline workflows. Well-designed layouts can save healthcare workers 1-2 hours per shift.
Infection Control Improvement
Analyze traffic patterns to minimize cross-contamination risks and optimize isolation protocols. Smart layouts reduce HAIs by 20-40%.
Cost Reduction
Reduce operational costs through better space utilization and improved workflows. Layout optimization can cut operational expenses by 15-25%.
Patient Experience
Create calming, navigable spaces that reduce anxiety and improve satisfaction scores. Good design directly impacts healing outcomes.
Regulatory Compliance
Ensure layouts meet ADA, OSHA, and accreditation standards. Proactive analysis prevents costly redesigns and compliance violations.
Healthcare Layout Analysis in Action
See how different healthcare facilities optimize their layouts for better outcomes
Emergency Department Flow Analysis
A regional medical center analyzed patient journey times from triage to discharge. By repositioning triage stations and creating dedicated fast-track areas, they reduced average wait times from 4.2 hours to 2.8 hours. The analysis revealed that 60% of delays occurred during patient handoffs between zones—a simple layout adjustment eliminated most bottlenecks.
ICU Workflow Optimization
A trauma center mapped nurse movement patterns during peak hours, discovering that staff walked an average of 6.8 miles per 12-hour shift. By relocating supply stations and medication rooms closer to patient beds, they reduced walking distance by 40% and increased bedside time by 90 minutes per nurse per shift.
Surgery Suite Efficiency Study
An orthopedic hospital analyzed turnover times between procedures, finding that equipment retrieval accounted for 35% of delays. Layout modifications to create procedure-specific staging areas reduced turnover time from 45 minutes to 28 minutes, allowing for one additional surgery per day per suite.
Pediatric Ward Safety Analysis
A children's hospital used heat mapping to identify high-traffic collision points where staff, families, and equipment intersected. Strategic placement of family lounges and play areas reduced hallway congestion by 50% and eliminated 80% of minor accidents involving mobile equipment.
Outpatient Clinic Patient Flow
A multi-specialty clinic analyzed patient movement from check-in to checkout, discovering that poor signage and confusing layouts caused 25% of patients to arrive late to appointments. Layout optimization and wayfinding improvements reduced late arrivals by 60% and improved patient satisfaction scores.
Pharmacy Layout for Medication Safety
A hospital pharmacy analyzed medication retrieval patterns and error rates, finding that similar-looking medications stored in adjacent locations caused 40% of near-miss events. Layout redesign based on usage frequency and visual differentiation reduced medication errors by 70%.
How Healthcare Layout Analysis Works
Transform your facility data into actionable design improvements
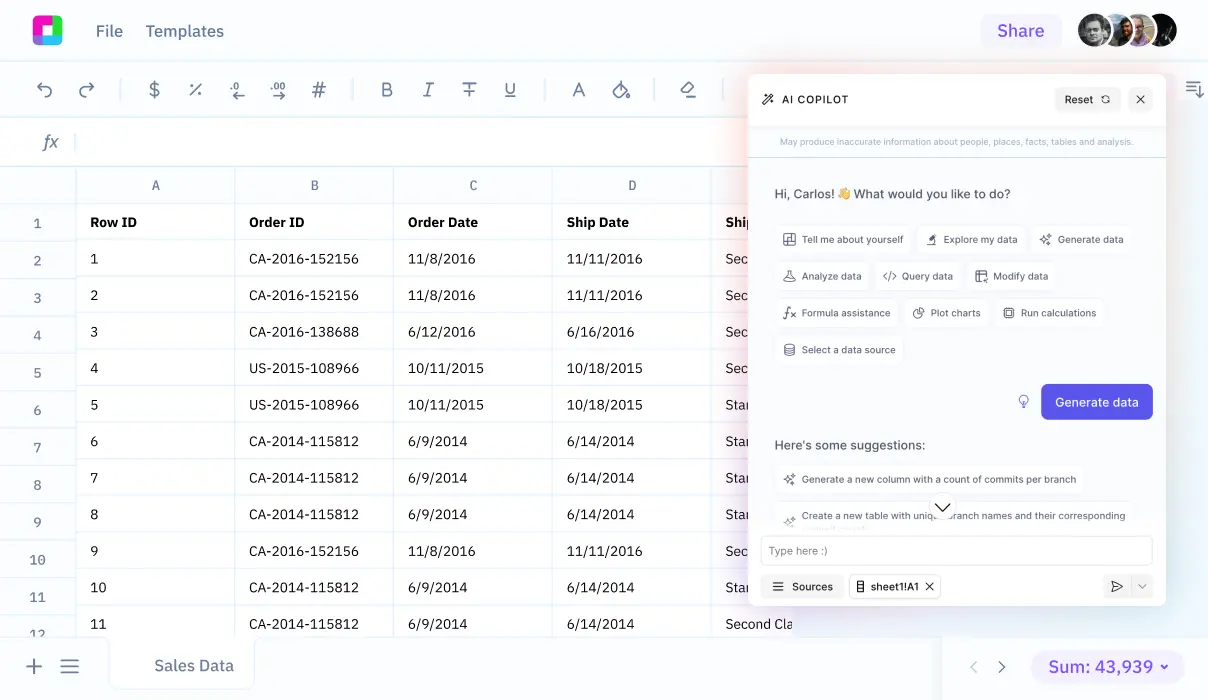
Data Collection & Import
Import floor plans, staff schedules, patient flow data, and equipment logs. Connect with existing HIMS, EHR systems, and badge tracking data. Sourcetable handles multiple data formats including CAD files, CSV exports, and real-time sensor feeds.
Traffic Pattern Analysis
Map movement patterns for staff, patients, visitors, and equipment. Identify bottlenecks, dead zones, and high-traffic intersections. Use AI to detect patterns that aren't obvious to human observers, like subtle workflow inefficiencies that compound over time.
Workflow Mapping
Trace patient journeys from admission to discharge, mapping every touchpoint and transition. Analyze task sequences, waiting times, and handoff locations. Identify where care delivery breaks down due to physical constraints.
Safety & Compliance Assessment
Evaluate sight lines for patient monitoring, assess fall risk zones, and check compliance with regulations. Analyze infection control protocols and identify opportunities to reduce cross-contamination through better layout design.
Optimization Recommendations
Generate specific, actionable recommendations for layout improvements. Prioritize changes by impact, cost, and implementation complexity. Create before-and-after scenarios to demonstrate expected outcomes.
Impact Measurement
Track key metrics before and after layout changes. Monitor patient satisfaction, staff efficiency, safety incidents, and operational costs. Build a continuous improvement cycle based on measurable results.
Essential Healthcare Layout Metrics
Successful healthcare layout analysis relies on tracking the right metrics. Here's what matters most:
Patient Flow Metrics
- Door-to-Provider Time: Average time from facility entry to first clinical contact
- Throughput Rate: Patients processed per hour during peak times
- Queue Length Analysis: Waiting room capacity vs. actual demand patterns
- Navigation Time: How long patients take to find destinations
Staff Efficiency Indicators
- Steps per Shift: Total walking distance for different roles
- Task Interruption Rate: How often workflows are disrupted by layout issues
- Equipment Retrieval Time: Average time to access needed supplies
- Communication Delays: Time lost due to poor sight lines or distance
Safety & Quality Measures
- Near-Miss Incidents: Close calls prevented by better design
- Patient Fall Locations: Mapping high-risk zones
- Code Response Times: Emergency team arrival speeds
- Infection Transmission Patterns: Disease spread correlation with layout
The beauty of comprehensive data analysis is how these metrics interconnect. Improving patient flow often enhances staff efficiency, which reduces errors, which improves patient satisfaction—a positive feedback loop that starts with smart layout decisions.
Advanced Analysis Techniques
Leverage cutting-edge tools to optimize your healthcare facility layout
Heat Mapping & Flow Visualization
Create visual representations of movement patterns, identifying hotspots and dead zones. Use color-coded overlays to spot optimization opportunities at a glance.
Predictive Modeling
Simulate layout changes before implementation. Model different scenarios to predict outcomes and ROI before committing to expensive renovations.
Real-Time Dashboard Monitoring
Track facility performance in real-time with live dashboards showing current bottlenecks, capacity utilization, and emerging issues.
Comparative Benchmarking
Compare your facility's performance against industry standards and similar institutions. Identify best practices and areas for improvement.
AI-Powered Pattern Recognition
Use machine learning to discover hidden patterns in complex facility data. Identify subtle correlations between layout and patient outcomes.
3D Visualization & Virtual Walkthroughs
Create immersive 3D models to test layout changes virtually. Walk through proposed designs before construction begins.
Frequently Asked Questions
How long does a comprehensive facility layout analysis take?
Timeline depends on facility size and complexity. A typical analysis takes 2-4 weeks for data collection and initial insights, with ongoing monitoring providing continuous optimization opportunities. Emergency departments and critical care units often show measurable improvements within the first week of implementation.
What data sources do I need for effective layout analysis?
Essential data includes floor plans, staff scheduling systems, patient flow logs, and equipment tracking. Optional but valuable sources include badge access data, nurse call logs, transport requests, and incident reports. Sourcetable integrates with most healthcare management systems to automate data collection.
Can layout analysis work for small clinics or just large hospitals?
Layout optimization benefits facilities of all sizes. Small clinics often see proportionally larger improvements because minor changes have major impact. Even a 3-room practice can reduce patient wait times and improve staff efficiency through smart layout analysis.
How do you measure ROI for layout optimization projects?
ROI calculations include reduced operational costs, improved staff productivity, decreased patient complaints, and better quality scores. Typical payback periods range from 6-18 months, with ongoing benefits including reduced liability, improved staff retention, and enhanced patient satisfaction scores.
What about compliance with healthcare regulations during layout changes?
Layout analysis includes comprehensive compliance checking against ADA, OSHA, Joint Commission, and local building codes. The analysis identifies opportunities that enhance compliance while improving efficiency, ensuring renovations meet all regulatory requirements.
How often should facility layouts be analyzed and updated?
Continuous monitoring provides the best results, with formal reviews quarterly or after major operational changes. Patient mix changes, new equipment, staffing adjustments, and service line additions all trigger layout reassessment needs.
Can layout analysis help with infection control protocols?
Absolutely. Layout analysis maps potential contamination pathways, identifies isolation protocol weaknesses, and optimizes hand hygiene station placement. During pandemic response, layout modifications based on data analysis significantly reduced transmission risks.
What's the difference between layout analysis and traditional facility planning?
Traditional planning relies on experience and best practices. Data-driven layout analysis uses actual facility performance data to identify specific problems and measure improvement outcomes. It's the difference between educated guessing and evidence-based decision making.
Getting Started with Layout Analysis
Ready to transform your healthcare facility? Here's your roadmap to success:
Phase 1: Baseline Assessment (Week 1-2)
Start by mapping your current state. Import existing floor plans, collect 2-3 weeks of operational data, and establish baseline metrics. Focus on high-impact areas like emergency departments, surgical suites, or patient registration areas where small improvements yield big results.
Phase 2: Data Analysis & Insights (Week 3-4)
Let the data tell the story. Use statistical analysis tools to identify patterns, bottlenecks, and optimization opportunities. Don't assume you know where the problems are—the data often reveals surprising inefficiencies.
Phase 3: Quick Wins (Week 5-6)
Implement low-cost, high-impact changes first. This might include relocating supply carts, adjusting furniture placement, or improving signage. These quick wins build momentum and demonstrate value to stakeholders.
Phase 4: Strategic Improvements (Month 2-3)
Tackle larger optimization projects based on your analysis findings. This phase might involve modest renovations, workflow redesigns, or technology implementations that address root causes identified in your data.
Phase 5: Continuous Monitoring (Ongoing)
Establish ongoing monitoring to track improvements and identify new optimization opportunities. Healthcare is dynamic—patient populations change, new services launch, regulations evolve. Your layout analysis should evolve too.
Remember: The goal isn't perfect layouts—it's continuously improving ones. Start with what you can measure, improve what matters most, and build a culture of data-driven facility optimization.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us