In the insurance industry, claims processing efficiency directly impacts customer satisfaction, operational costs, and regulatory compliance. A single percentage point improvement in processing speed can translate to millions in cost savings for large insurers, while faster resolution times build customer loyalty and reduce administrative overhead.
Claims processing efficiency analysis examines every stage of the claims lifecycle - from initial submission to final payout. By analyzing processing times, approval rates, rework frequencies, and resource allocation, insurers can identify optimization opportunities that deliver measurable business impact.
Why Claims Processing Analysis Matters
Discover how efficiency analysis transforms insurance operations and drives competitive advantage.
Reduce Processing Time
Identify bottlenecks that slow claim resolution. Typical improvements range from 15-40% reduction in average processing time through workflow optimization.
Lower Operational Costs
Streamline resource allocation and eliminate redundant processes. Most insurers see 10-25% reduction in claims processing costs within the first year.
Improve Accuracy
Reduce errors and rework through better process visibility. Enhanced accuracy leads to fewer disputes and improved customer satisfaction scores.
Enhance Compliance
Monitor regulatory adherence and audit trails automatically. Ensure consistent compliance with industry standards and reporting requirements.
Boost Customer Satisfaction
Faster, more transparent claims processing improves customer experience. Studies show 30% improvement in satisfaction scores with optimized processes.
Data-Driven Decisions
Make informed process improvements based on actual performance data rather than assumptions. Track the impact of changes in real-time.
Real-World Claims Processing Analysis Examples
Auto Insurance Claims Workflow Analysis
A regional auto insurer analyzed their claims processing workflow and discovered that 60% of delays occurred during the damage assessment phase. The analysis revealed:
Property Claims Processing Efficiency Study
A property insurance company conducted efficiency analysis across three regional offices to standardize best practices:
Health Insurance Claims Processing Analysis
A health insurance provider analyzed their claims processing to improve member experience and reduce administrative costs:
The analysis led to implementation of automated pre-screening rules, which reduced simple claim processing to 0.8 days and decreased error rates to 6.2%.
How Claims Processing Analysis Works
Follow our systematic approach to analyze and optimize your claims processing workflow.
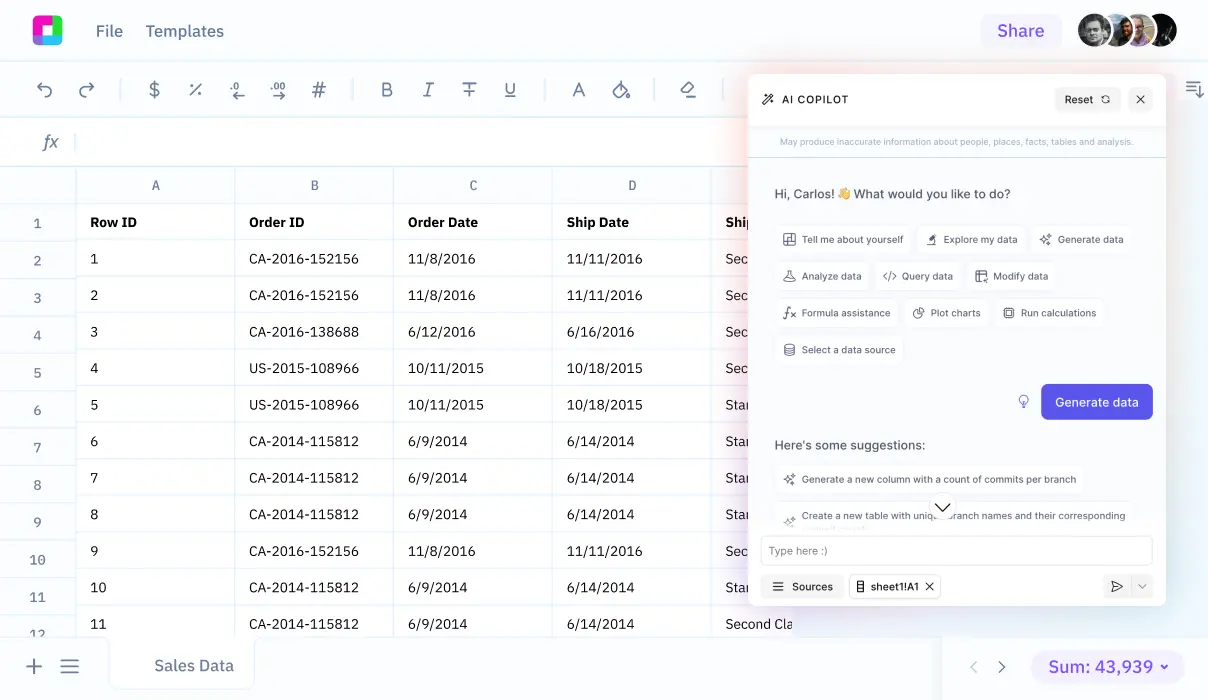
Data Collection
Gather claims processing data from your systems including timestamps, status changes, adjuster assignments, and resolution details. Import from multiple sources seamlessly.
Process Mapping
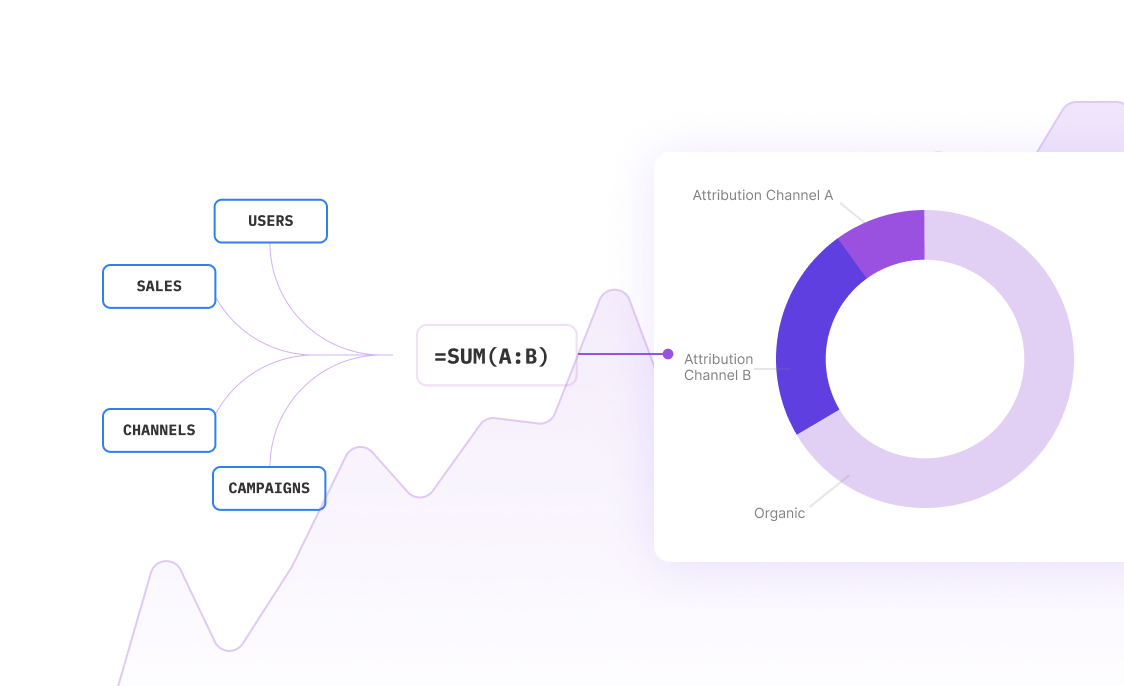
Visualize your current claims workflow from submission to payout. Identify all touchpoints, decision points, and handoffs between departments or systems.
Performance Measurement
Calculate key metrics like average processing time, first-pass resolution rate, cost per claim, and customer satisfaction scores across different claim types.
Bottleneck Identification
Pinpoint where delays occur most frequently. Analyze queue times, approval delays, and resource constraints that impact processing speed.
Root Cause Analysis
Dig deeper into identified bottlenecks to understand underlying causes. Examine staffing levels, system limitations, and process inefficiencies.
Optimization Recommendations
Generate specific, actionable recommendations for process improvements. Prioritize changes based on potential impact and implementation difficulty.
Claims Processing Analysis Applications
Explore how different types of insurers use processing efficiency analysis to improve operations.
Multi-Line Insurance Companies
Analyze processing efficiency across auto, home, and commercial lines. Compare performance between product lines and identify best practices for cross-training and resource allocation.
Property & Casualty Insurers
Focus on catastrophic claims processing and seasonal volume fluctuations. Optimize staffing models and vendor management for large-scale events.
Health Insurance Providers
Streamline medical claims processing with emphasis on prior authorization workflows, provider network efficiency, and member communication protocols.
Workers' Compensation Carriers
Analyze complex claims requiring medical management, return-to-work coordination, and legal compliance. Focus on long-term claim cost management.
Specialty Insurance Markets
Optimize processing for unique coverage types requiring specialized knowledge. Balance expertise requirements with processing speed goals.
Insurance Adjusting Firms
Analyze adjuster productivity, territory management, and client satisfaction. Optimize scheduling and workload distribution across field staff.
Essential Claims Processing Metrics
Effective claims processing analysis relies on tracking the right metrics. Here are the most critical indicators for measuring and improving efficiency:
Time-Based Metrics
Quality Metrics
Cost and Productivity Metrics
Customer Experience Metrics
Frequently Asked Questions
How long does it take to see results from claims processing analysis?
Initial insights typically emerge within 2-4 weeks of data collection. Process improvements can begin implementation immediately, with measurable results often visible within 60-90 days. Full optimization benefits usually materialize over 6-12 months as new processes become established.
What data sources are needed for comprehensive analysis?
Essential data includes claims management system records, adjuster activity logs, customer communication timestamps, payment processing records, and quality audit results. Integration with policy administration systems and customer service platforms provides additional context for holistic analysis.
How do you handle claims processing analysis for multiple lines of business?
Multi-line analysis requires segmentation by product type while identifying cross-line opportunities. We analyze each line individually to respect unique workflows, then examine shared resources, common bottlenecks, and standardization opportunities that benefit overall efficiency.
Can claims processing analysis help with regulatory compliance?
Absolutely. Analysis identifies compliance gaps, tracks regulatory metrics like response times and settlement timeframes, and creates audit trails for regulatory reporting. Many clients use ongoing analysis to demonstrate compliance improvements to regulators and maintain certification requirements.
What's the typical ROI for claims processing optimization projects?
Most insurers see 15-30% reduction in processing costs within the first year, translating to ROI of 200-400%. Benefits include reduced labor costs, fewer errors requiring rework, improved customer retention, and increased adjuster productivity. Larger organizations often see seven-figure annual savings.
How do you measure success in claims processing efficiency projects?
Success metrics include reduced average processing time, improved first-pass resolution rates, lower cost per claim, increased customer satisfaction scores, and enhanced regulatory compliance. We establish baseline measurements and track improvements monthly to ensure sustained progress.
Can analysis help with catastrophic claims processing?
Yes, catastrophic event analysis is crucial for large-scale claims management. We analyze surge capacity planning, vendor management efficiency, resource allocation during peak periods, and communication protocols. This helps insurers prepare for future events and maintain service levels during crisis periods.
How does technology integration affect claims processing analysis?
Technology integration is essential for modern claims processing. Analysis examines API performance, system integration efficiency, automation rates, and user adoption of new technologies. We help identify which technologies provide the best efficiency gains and guide implementation strategies.
Frequently Asked Questions
If your question is not covered here, you can contact our team.
Contact Us